Session Information
Date: Monday, November 9, 2015
Title: Epidemiology and Public Health III: Risk Factors, Treatment and Outcomes of Gout and OA
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose:
Obesity is one of the few modifiable risk factors of knee
osteoarthritis (OA). However, it is not established whether a mechanical or
metabolic mechanism is more important for the development of knee OA. Central adiposity contributes more than peripheral adiposity to cardiometabolic diseases, while analogous associations with knee OA
are not known. The aim of this study was to examine the
associations of 1) total body fat mass and appendicular lean mass, 2) abdominal
subcutaneous adipose tissue (SAT) and 3) visceral adipose tissue (VAT) with
knee structural changes in community-dwelling older adults.
Methods:
A subsample (n=866,
mean age 73.5±2.9,
525 women, 46% black) of the Health, Aging, Body
Composition Study participants (n=3,075, mean age 73.6, 52% women, 42% black)
was included in this analysis. Body composition was assessed at baseline using whole
body DXA, and abdominal SAT area and VAT area (cm2)
were calculated from a single 10 mm thickness abdominal CT. Knee MRI images
were obtained using a 1.5T system at the year 2 or
year 3 visit and assessed using the Whole-Organ Magnetic Resonance
Imaging Score (WORMS). The presence of any bone marrow lesion (BMLs, grade
≥1), cartilage damage (≥2), meniscus damage (≥1) and synovitis/effusion
(≥1) was examined. The associations of body composition or adipose tissue
measures with the knee outcomes were examined using logistic regression models stratified
by sex. Total body fat mass and appendicular lean mass were entered in models
simultaneously. VAT and SAT divided by body weight (cm2/kg) were
entered in separate models. In the final models, age, race, height, study site,
education, history of knee injury, knee pain, smoking status, alcohol drinking,
total physical activity, time spent watching TV and use of NSAIDs at baseline
were adjusted. Correlation of knees within person was taken into account by
generalized estimating equations.
Results:
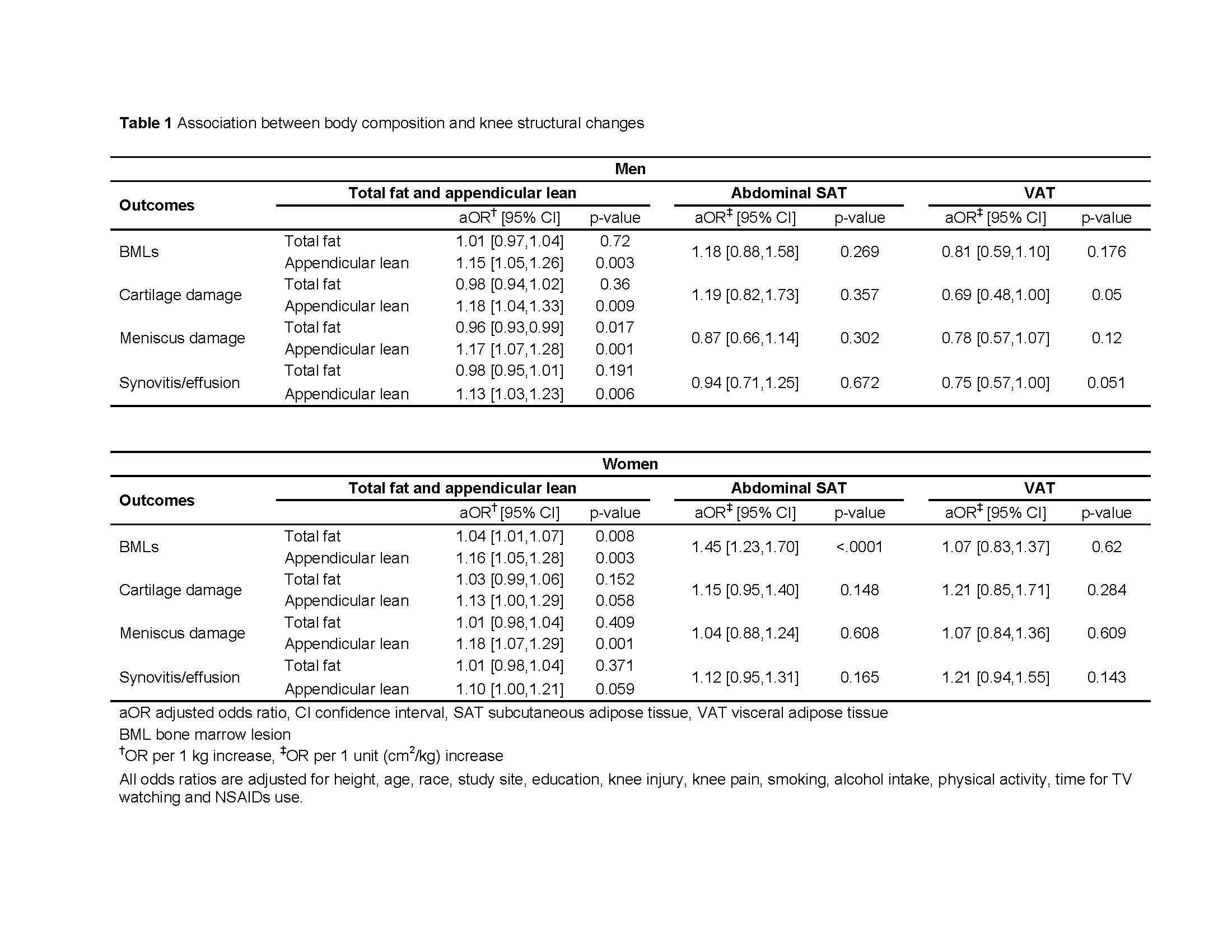
In an analysis of 1,413 knees, higher
appendicular lean mass was associated with higher odds of all knee MRI outcomes,
but higher total body fat mass was associated only with lower odds of meniscus
damage in men (Table 1). In women, higher appendicular lean mass was associated
with BMLs and meniscus damage. Total body fat mass was also associated with
BMLs, but the adjusted odds ratio was smaller than lean mass. Abdominal SAT or
VAT were not significantly associated with any of the knee MRI outcomes in men.
In women, higher abdominal SAT was associated with higher odds of BMLs, but no
association was found for VAT.
Conclusion:
The stronger association between
knee MRI outcomes and lean mass compared to total fat mass and the lack of the
association with VAT suggest the importance of overall higher weight rather
than total fat or central adiposity specifically for knee structural changes.
This could indicate a mechanical rather than a metabolic pathway.
To cite this abstract in AMA style:
Fujii T, Miljkovic I, Boudreau RM, Guermazi A, Piva SR, Strotmeyer ES, Carbone L, Harris TB, Marques EA, Shea MK, Nevitt MC, Newman AB, Kwoh CK. Are General and Central Adiposity Associated with MRI-Assessed Structural Changes in the Knees of Older Adults? [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/are-general-and-central-adiposity-associated-with-mri-assessed-structural-changes-in-the-knees-of-older-adults/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/are-general-and-central-adiposity-associated-with-mri-assessed-structural-changes-in-the-knees-of-older-adults/