Session Information
Date: Monday, October 22, 2018
Title: Spondyloarthritis Including Psoriatic Arthritis – Clinical Poster II: Clinical/Epidemiology Studies
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The interval from symptom onset till diagnosis in axial spondyloarthritis (axSpA) was reported a decade ago to be between five and ten years. The objective of this study was to explore if the diagnostic delay has improved over the past years and to analyse factors associated with the delay.
Methods: A sample of persons with axSpA (ICD-10 M45) stratified by age and sex was drawn from claims data of a large nationwide statutory health insurance fund in Germany. Each person in the sample received in 2015 a questionnaire gathering information on demographic, disease-related and socioeconomic characteristics. Disease-related parameters comprised the date of first symptoms, the date of diagnosis, the HLA-B27 status as well as the presence of extra-articular manifestations (uveitis, psoriasis, chronic-inflammatory bowel disease). Multivariable linear regression analysis was used to analyse factors associated with the diagnostic delay.
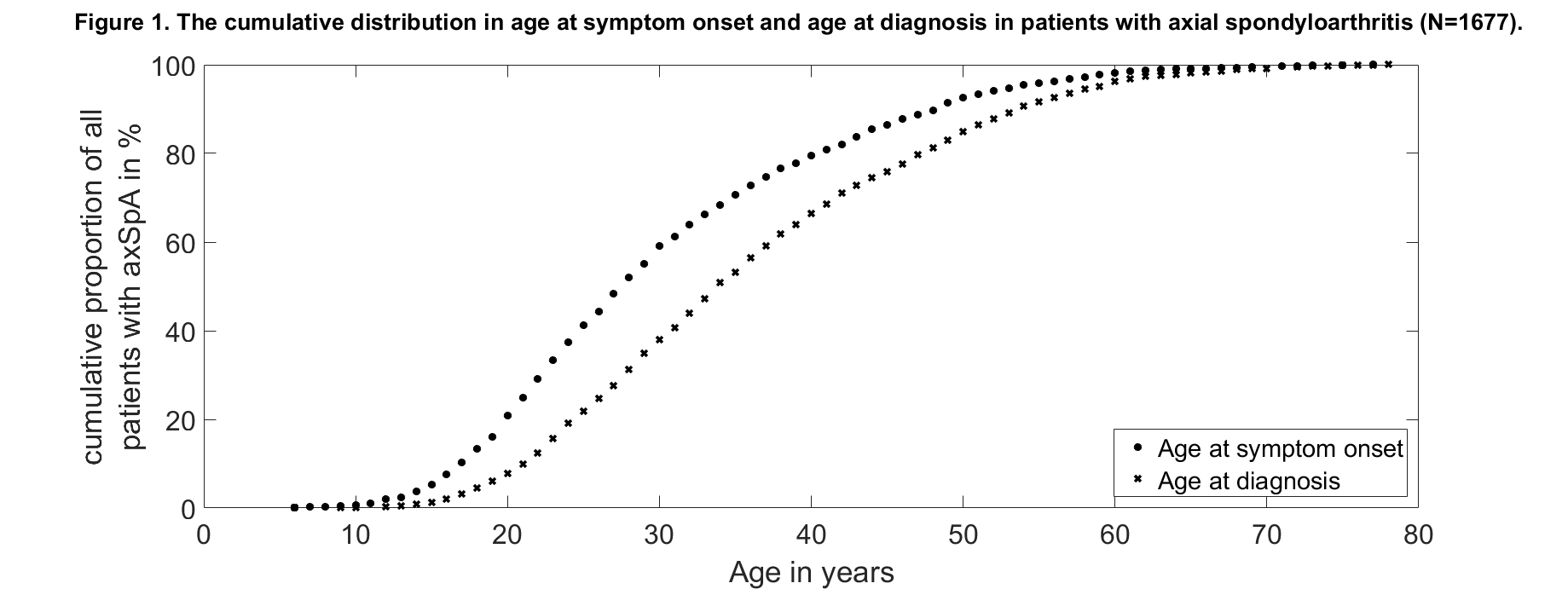
Results: A total of 1,677 persons with axSpA were included in the analysis. The mean age was 56 years and 46% were female. The mean (95% confidence interval [CI]) diagnostic delay in the whole group was 5.7 (5.4 – 6.0) years and the median was 2.3 years (Fig. 1). Overall, 407 persons were diagnosed between 1996 and 2005 and 484 persons between 2006 and 2015. The diagnostic delay was not substantially different in both periods: For patients diagnosed between 1996 and 2005 the mean (95% CI) diagnostic delay was 6.3 (5.6 – 7.0) years and the median was 2.6 years. For patients diagnosed between 2006 and 2015 the mean (95% CI) diagnostic delay was 7.4 (6.6 – 8.1) years and the median was 2.7 years. Persons with a long diagnostic delay were more often female and had less often a positive HLA-B27 status compared to persons with a short diagnostic delay (Tab. 1). Multivariable linear regression revealed that female sex, negative HLA-B27 status, prevalence of psoriasis and younger age at symptom onset are factors associated with a longer diagnostic delay (Tab. 2).
Conclusion: The mean diagnostic delay of about 7 years represents currently one of the major challenges in field of SpA. Female sex, negative HLA-B27 status, presence of psoriasis and younger age at symptom onset had a negative impact on the diagnostic delay.
|
Table 1. Main demographic, disease-related, lifestyle and socioeconomic characteristics of patients with axSpA stratified by the delay to diagnosis. |
||||
|
|
Total
N=1677 |
Delay to diagnosis <2.3 years N=814 |
Delay to diagnosis ≥2.3 years N=863 |
P value |
|
Sex, female |
45.9 |
40.6 |
50.8 |
<0.0001 |
|
Age, years |
55.9 ± 0.1 |
54.3 ± 0.3 |
57.3 ± 0.3 |
<0.0001 |
|
Age at symptom onset, years |
30.6 ± 0.3 |
33.1 ± 0.4 |
28.3 ± 0.3 |
<0.0001 |
|
Age at diagnosis, years |
36.3 ± 0.3 |
33.8 ± 0.4 |
38.6 ± 0.4 |
<0.0001 |
|
HLA-B27 (+) |
86.3 |
89.2 |
83.8 |
0.0103 |
|
BASDAI*, 0-10 |
4.5 ± 0 |
4.3 ± 0.1 |
4.7 ± 0.1 |
0.0002 |
|
BASFI*, 0-10 |
4.1 ± 0.1 |
3.8 ± 0.1 |
4.4 ± 0.1 |
<0.0001 |
|
Swollen/tender joints, 0-44 |
7 ± 0.2 |
6.6 ± 0.3 |
7.4 ± 0.3 |
0.1065 |
|
WHO-5 *, 0-100 |
45 ± 0.5 |
46.8 ± 0.7 |
43.3 ± 0.7 |
0.0012 |
|
Inflammatory bowel disease, ever |
9 |
9.6 |
8.5 |
0.4481 |
|
Uveitis, ever |
27.8 |
26.4 |
29.1 |
0.2347 |
|
Psoriasis, ever |
15.1 |
13.9 |
16.2 |
0.2000 |
|
Educational level |
|
|
|
0.0057 |
|
low |
29.1 |
31.9 |
26.6 |
|
|
middle |
42.8 |
38.8 |
46.4 |
|
|
high |
28.1 |
29.3 |
27 |
|
|
Smoking, current* |
19 |
20 |
18.1 |
0.3454 |
|
Pharmacological treatment* |
|
|
|
|
|
NSAIDs |
58.9 |
56.7 |
60.9 |
0.0883 |
|
non-opioid analgesics |
22.2 |
20.3 |
24 |
0.0692 |
|
opioids |
15.4 |
14 |
16.8 |
0.1265 |
|
bDMARDs |
17.5 |
15.7 |
19.1 |
0.0609 |
|
csDMARDs |
11.5 |
12.7 |
10.4 |
0.1403 |
|
steroids |
19.5 |
18.7 |
20.2 |
0.4357 |
|
No pharmacological treatment* |
22.5 |
25.1 |
20 |
0.0148 |
|
*referring to the time of questionnaire, not the time of diagnosis. Values are presented as mean ± standard error of the mean for continuous characteristics and as percentages otherwise. P-values were assessed using analyses of variance for continuous characteristics and Rao-Scott chi-square tests otherwise. WHO-5, 5-item World Health Organization Well-Being Index; BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath Ankylosing Spondylitis Functional Index, NSAIDs, Nonsteroidal Anti-Inflammatory Drugs; csDMARDs, conventional synthetic Disease-Modifying Anti-Rheumatic Drugs; bDMARDs, biological Disease-Modifying Anti-Rheumatic Drugs. |
||||
|
Table 2. Factors associated with diagnostic delay: results from multivariable linear regression analysis. |
||
|
|
Reference |
Estimate (95% CI) |
|
Sex, female |
male |
1.85 (1.06, 2.65) |
|
Age at symptom onset |
per 10 years |
-1.91 ( -2.29 , -1.53 ) |
|
HLA-B27 status, positive |
negative |
-3.61 (-5.14 , -2.07) |
|
Psoriasis, yes |
no |
1.4 (0.08 , 2.73) |
|
CI, Confidence Interval |
||
To cite this abstract in AMA style:
Redeker I, Callhoff J, Hoffmann F, Haibel H, Sieper J, Zink A, Poddubnyy D. Which Factors Influence the Diagnostic Delay in Patients with Axial Spondyloarthritis? [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/which-factors-influence-the-diagnostic-delay-in-patients-with-axial-spondyloarthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/which-factors-influence-the-diagnostic-delay-in-patients-with-axial-spondyloarthritis/