Session Information
Date: Tuesday, November 9, 2021
Title: Pediatric Rheumatology – Clinical Poster III: Miscellaneous Rheumatic Disease (1614–1644)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Although COVID-19 has been less severe in the pediatric population, with cases more likely to be mild or asymptomatic, there remains a proportion of pediatric cases with features of cytokine storm syndrome (CSS), leading to hyperinflammation, uncontrolled immune activation, respiratory disease, and end-organ failure. Additionally, multisystem inflammatory syndrome in children (MIS-C) has emerged as a relatively rare post-infectious sequela of COVID-19 with similar hyperinflammation, severe shock, and organ dysfunction. Prior to and during the COVID-19 pandemic, scoring systems have been developed and used to identify patients at risk for CSS. Our study explores the utility of existing CSS, macrophage activation syndrome (MAS), and hemophagocytic lymphohistiocytosis (HLH) scoring systems in identifying pediatric patients at risk for CSS in the setting of MIS-C and COVID-19.
Methods: Pediatric patients with MIS-C and active COVID-19 infection at a single institution were identified. Infectious data, clinical findings, and laboratory values were collected, and patients were stratified by disease severity into mild MIS-C, severe MIS-C, and severe COVID-19, dependent on symptomology, positive COVID-19 polymerase chain reaction (PCR) or serology, and need for vasopressor and/or ventilatory support. Eight historically utile scoring systems for MAS, HLH, and CSS were used to examine the cohort of MIS-C and pediatric COVID-19 patients for features and diagnosis of cytokine storm.
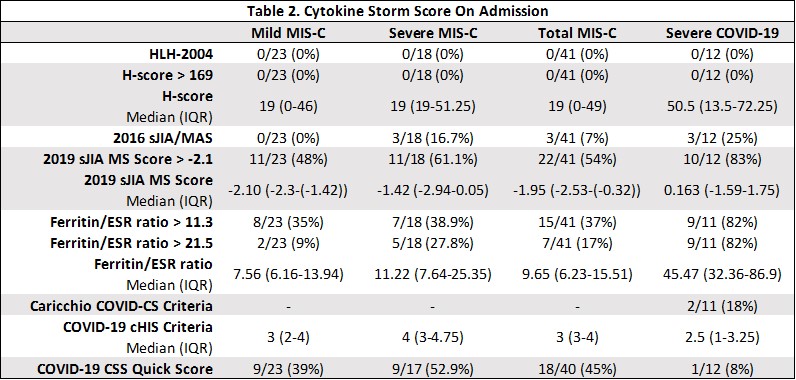
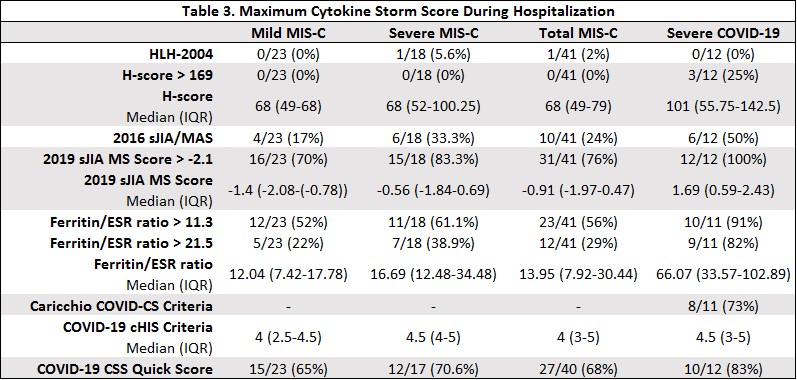
Results: 23 patients with mild MIS-C, 18 patients with severe MIS-C, and 12 patients with severe COVID-19 were identified. The HLH-2004 and HScore scoring systems did not identify any MIS-C or COVID-19 patients as having CSS on admission to the hospital, with only one MIS-C patient meeting HLH-2004 criteria and three patients meeting HScore criteria at peak disease severity during hospitalization. The 2016 sJIA/MAS criteria, ferritin/ESR ratio, and COVID-19 CSS Quick Score identified CSS in more patients and was more useful in distinguishing between COVID-19 and MIS-C hyperinflammation and severity. The 2019 MS Score and COVID-19 cHIS criteria were less helpful, as the MS score likely overestimated CSS due to use of headache as a feature of its criteria, and the cHIS resulted in similar scores across the board regardless of severity or disease. The Caricchio COVID-CS did well in identifying CSS in pediatric COVID-19, but was less useful in MIS-C due to its COVID-19 specific criteria.
Conclusion: MIS-C and pediatric COVID-19 result in relatively unique cytokine storm syndromes and patterns of inflammation. Existing scoring systems for cytokine storm syndromes likely do not capture the full breadth of this disease process in MIS-C and pediatric COVID-19.
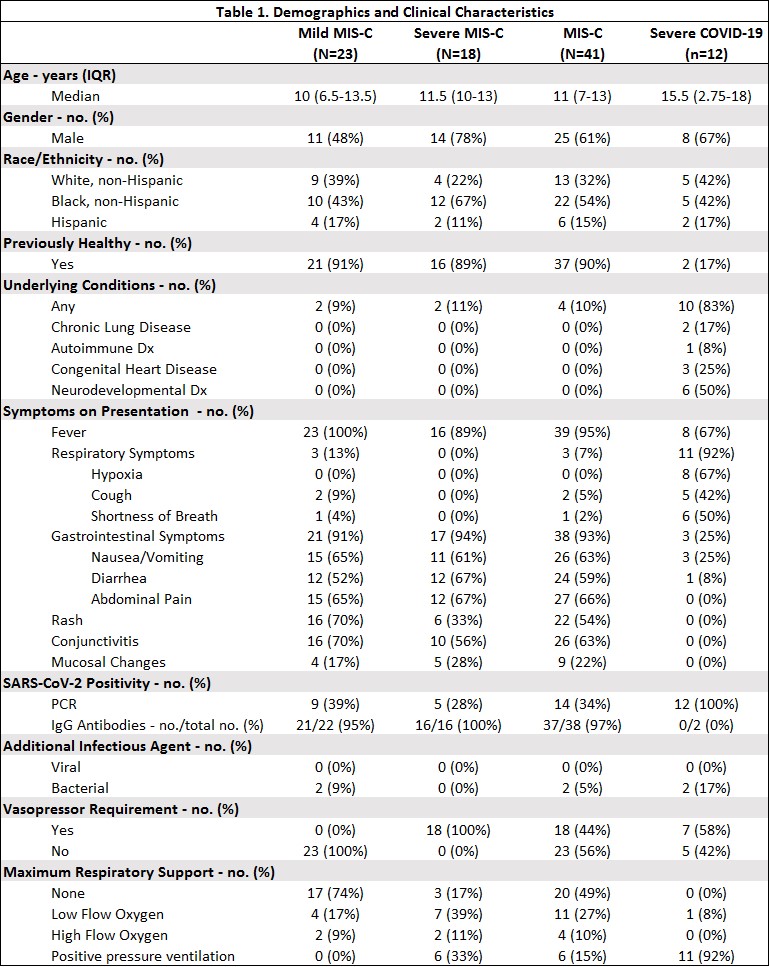 Demographics and Clinical Characteristics of Patient Population
Demographics and Clinical Characteristics of Patient Population
To cite this abstract in AMA style:
Cron R, Reiff D. Where Do Multisystem Inflammatory Syndrome in Children (MIS-C) and Pediatric COVID-19 Fit Under the Cytokine Storm Syndrome Umbrella? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/where-do-multisystem-inflammatory-syndrome-in-children-mis-c-and-pediatric-covid-19-fit-under-the-cytokine-storm-syndrome-umbrella/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/where-do-multisystem-inflammatory-syndrome-in-children-mis-c-and-pediatric-covid-19-fit-under-the-cytokine-storm-syndrome-umbrella/