Session Information
Date: Tuesday, November 15, 2016
Title: Epidemiology and Public Health II: Obesity, Cancer and Mortality
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose : Weight loss may explain the obesity paradox for mortality, since those who unintentionally lose weight to reach normal BMI may have higher mortality than those with obesity and stable weight. A prior study among RA patients found an association between weight loss and increased mortality. However, weight was examined close to time of death in established RA without a non-RA comparison so the findings may not be specific to RA. Therefore, we investigated the association of weight change in the early RA period with subsequent mortality, and included a matched non-RA group to evaluate the influence of RA.
Methods : We identified incident RA by 1987 ACR criteria during follow-up of the Nurses’ Health Study (1976-2012) to form a cohort followed before and after RA onset. We created a comparison cohort by matching RA cases to non-RA comparators by age and year at the index date of RA diagnosis. Anthropometric, behavioral, and clinical data were collected through biennial questionnaires. To capture the entire early RA period, weight change was defined as the difference between weight at 4 years before and 4 years after RA diagnosis (“peri-RA”) or index date (“peri-index”). We used Cox regression to estimate HRs for mortality by weight change categories separately in each cohort. We combined both cohorts to evaluate the RA-specific effect and weight change on mortality.
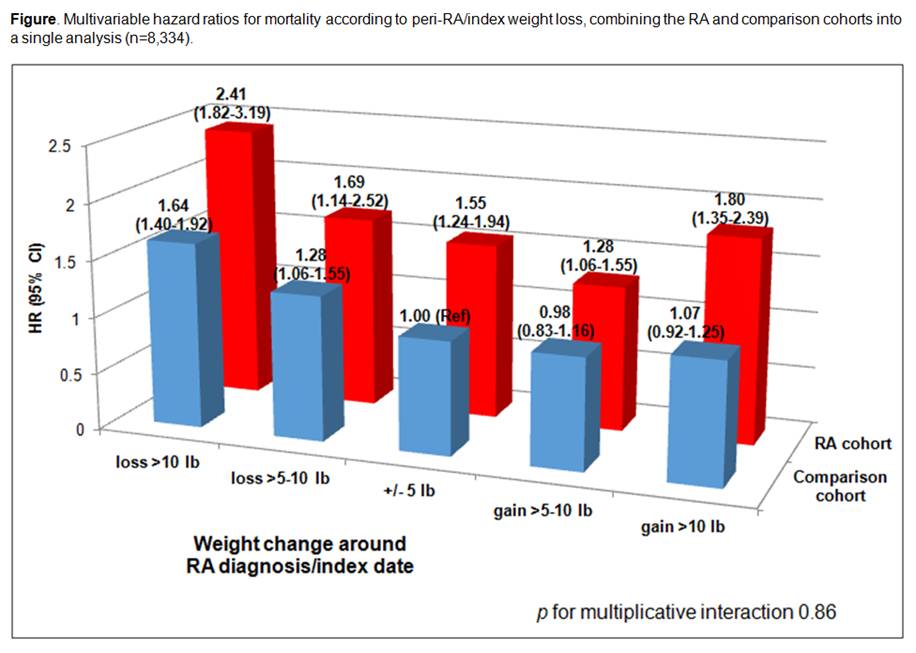
Results : Among 121,700 women, we identified 875 subjects with incident RA, matched to 7,459 non-RA comparators. In the RA cohort, 16.2% lost >10 lbs peri-RA; 12.1% of comparators had weight loss >10 lbs peri-index. There were 243 (27.8%) deaths in the RA cohort and 1,369 (18.4%) deaths among comparators. After adjustment for BMI, smoking, diet, physical activity, comorbidities (cancer, CVD, and diabetes), erosions, serostatus, and nodules, weight loss >10 lbs peri-RA had HR for mortality of 1.61 (95%CI 1.12-2.32, Table), identical to the comparison cohort (HR 1.61, 95%CI 1.38-1.89). Weight gain was not significantly associated with mortality in either cohort. When combining both cohorts, RA had higher absolute mortality risk, but there was no interaction between RA or comparators with weight change for mortality (pint=0.86, Figure).
Conclusion : In this large prospective study with up to 36 years of follow-up, weight loss around RA diagnosis increased subsequent mortality risk among women. We found similar results in non-RA comparators and evaluated weight change in the early RA period when disease-specific processes are most likely to contribute to weight loss or gain. Therefore, an obesity paradox for mortality may occur in the general population but is not specifically related to RA. 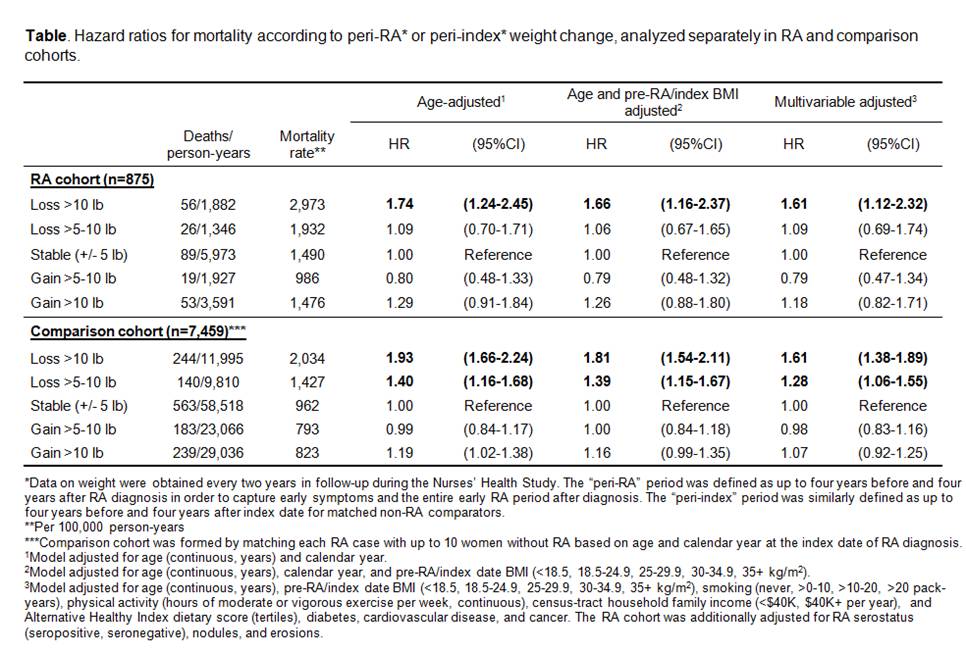
To cite this abstract in AMA style:
Sparks JA, Chang SC, Nguyen USDT, Barbhaiya M, Tedeschi SK, Lu B, Costenbader KH, Zhang Y, Choi HK, Karlson EW. Weight Loss in the Early Rheumatoid Arthritis Period Is Associated with Subsequent Increased Mortality in RA Patients and Matched Comparators: Evidence Against an RA-Specific Obesity Paradox [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/weight-loss-in-the-early-rheumatoid-arthritis-period-is-associated-with-subsequent-increased-mortality-in-ra-patients-and-matched-comparators-evidence-against-an-ra-specific-obesity-paradox/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/weight-loss-in-the-early-rheumatoid-arthritis-period-is-associated-with-subsequent-increased-mortality-in-ra-patients-and-matched-comparators-evidence-against-an-ra-specific-obesity-paradox/
