Session Information
Session Type: Plenary Session
Session Time: 11:30AM-1:00PM
Background/Purpose: Vitamin K is an essential co-factor in the post-translational gamma-carboxylation of glutamic acid to form gamma-carboxy-glutamic acid (Gla) residues. This confers functionality to vitamin K-dependent proteins including those in bone and cartilage that play an important role in regulating mineralization. Low vitamin K can lead to under-carboxylation of Gla proteins and thus their dysfunction. Vitamin K deficiency has been associated with OA, and a randomized trial of vitamin K supplementation demonstrated trends towards less OA progression. Studies to date have not evaluated whether vitamin K antagonism with warfarin can be detrimental to OA. We therefore evaluated the relation of warfarin to risk of knee and hip replacements as a reflection of end-stage OA.
Methods: We conducted a nested case-control study using The Health Improvement Network, a general practitioner (GP)-based electronic medical records database from the UK that is representative of the general population. To minimize confounding by indication, we limited our study sample to adults (aged 40-89) with atrial fibrillation, as this diagnosis warrants therapy with anticoagulation. Additionally, we compared warfarin, a vitamin K antagonist, with direct oral anticoagulants (DOAC), which are not vitamin K antagonists. Because DOACs were first marketed in the UK in 2008, we limited our study to those who had been enrolled for ≥1 year with a GP between 2009 and 2018. We excluded individuals with knee or hip replacement (KR/HR) prior to 2014, severe co-morbidities that would limit surgery, those with warfarin or DOAC use within 1 year prior to our study period, and those who used both drugs during study period. We identified cases as those with KR or HR between 2014-2018, with surgery date being the index date for cases. Each case was matched with up to 4 controls by age and gender. We defined warfarin and DOAC use as having ≥1 prescription after study entry and within 1 year prior to the index date. We assessed the relation of warfarin compared with DOAC use to risk of KR or HR using conditional logistic regression, adjusting for potential confounders.
Results: We identified 913 subjects with KR or HR (cases) who were age and gender-matched 4:1 with 3652 controls (mean age 74, 46% female). Of the 913 cases, 64.9% were warfarin users while 35.1% were DOAC users; in contrast, of the 3652 controls, 56.3% were warfarin users while 43.6% were DOAC users. With adjustment for potential confounders, warfarin users had 1.57 times higher odds of KR or HR than DOAC users (Adjusted OR 1.57, 95% CI (1.30-1.89)) (Table). When matched by practice ID to account for practice variation, we found a slightly diminished but significant association (Adjusted OR 1.25, 95% CI (1.03-1.52)). There was increasing risk of KR or HR with duration of warfarin vs. DOAC exposure (Figure).
Conclusion: Warfarin use, a vitamin K antagonist, was associated with significantly greater risk of KR or HR (an indicator for end-stage knee OA) than DOAC use, with risk increasing with duration of use. These data add further support to the importance of adequate vitamin K and its dependent proteins in limiting progression of OA and raises the consideration of using DOACs over warfarin when indicated in those with or at risk of OA.
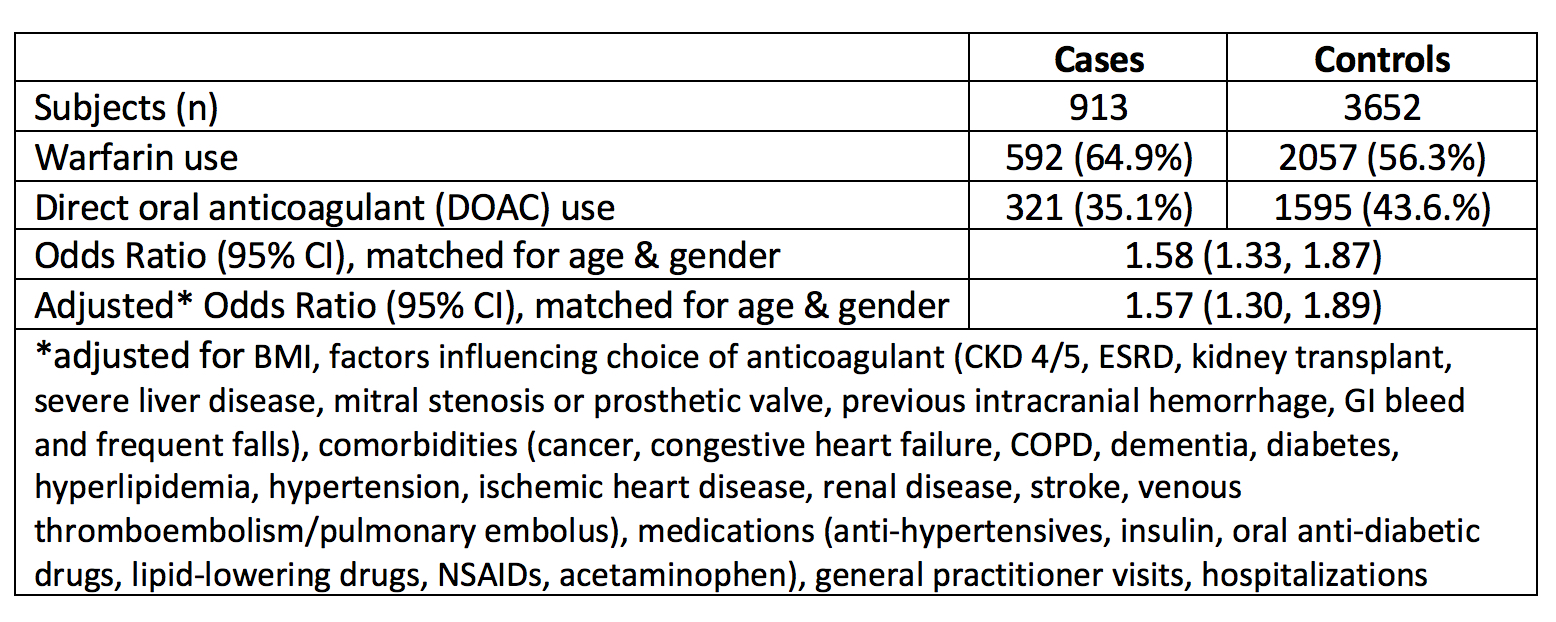 Table: Relation of Warfarin versus DOAC use to Risk of Knee or Hip Replacement
Table: Relation of Warfarin versus DOAC use to Risk of Knee or Hip Replacement
 Figure: Relation of Duration of Anti coagulation use (warfarin vs. DOAC) to Risk of KR or HR
Figure: Relation of Duration of Anti coagulation use (warfarin vs. DOAC) to Risk of KR or HR
To cite this abstract in AMA style:
Ballal P, Peloquin C, Boer C, Neogi T. Warfarin Use and Risk of Knee and Hip Replacements [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/warfarin-use-and-risk-of-knee-and-hip-replacements/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/warfarin-use-and-risk-of-knee-and-hip-replacements/
