Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Animal model studies have demonstrated the significant role of inflammation in the pathogenesis of osteoarthritis (OA) and of pain. Visceral fat, rather than subcutaneous fat, is a major source of proinflammatory cytokines and adipokines. In this study, we examined whether amount of visceral fat was associated with the risk of knee OA or musculoskeletal pain.
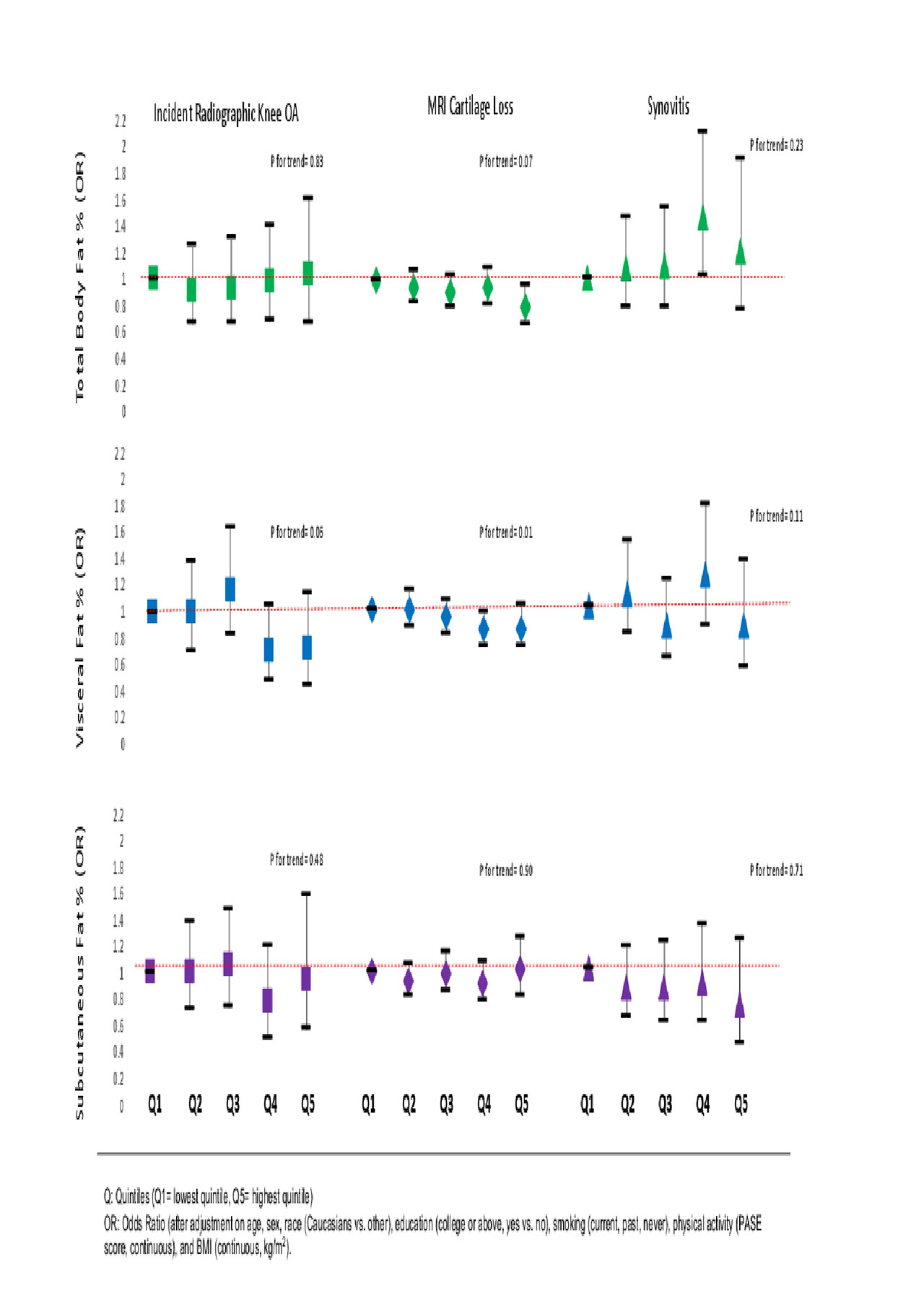
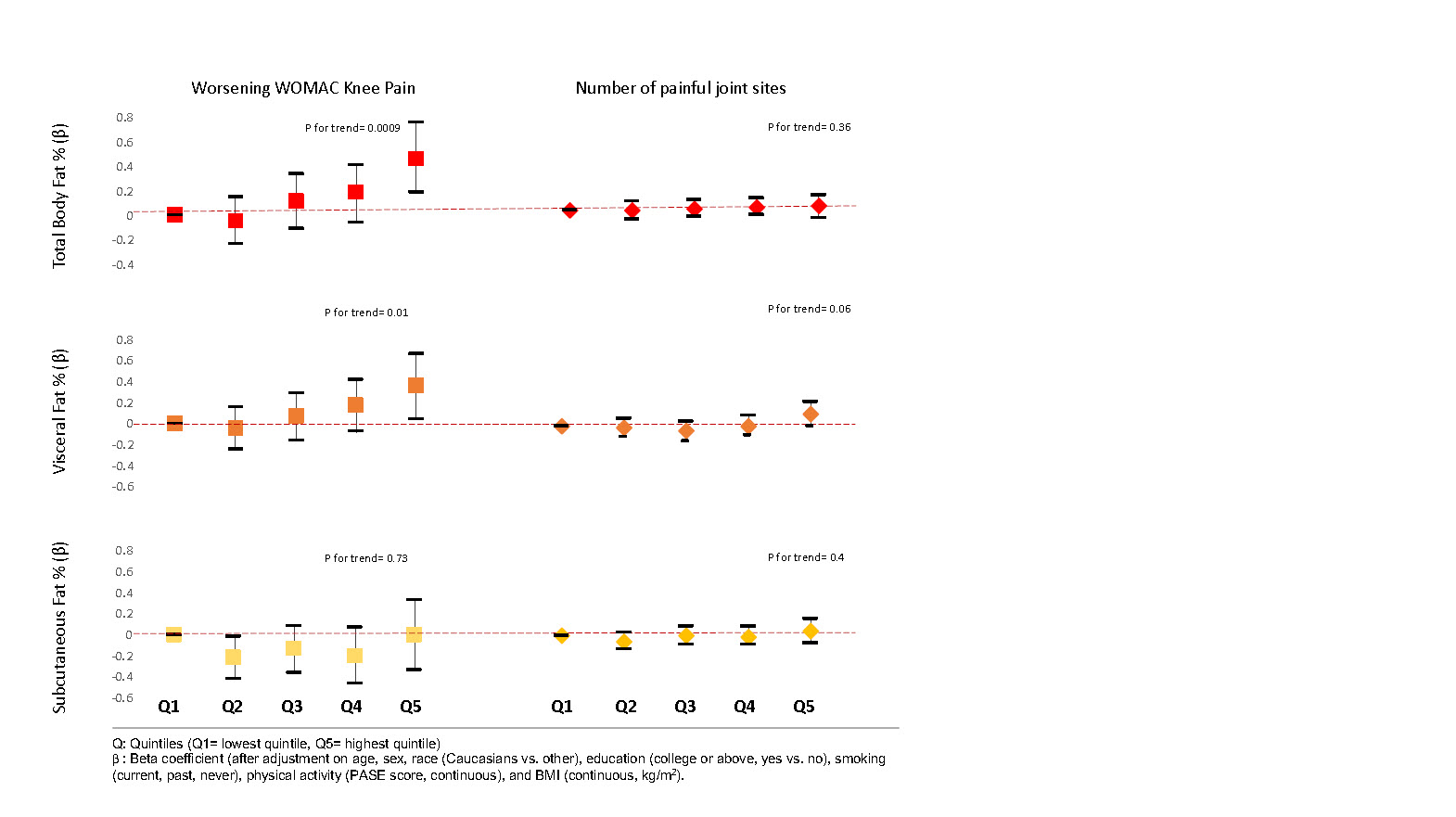
Methods: Participants in the Multicenter Osteoarthritis Study (MOST), a NIH funded longitudinal cohort study of persons at risk of or with knee OA underwent whole body dual energy x-ray absorptiometry (DEXA) scans at baseline that were assessed for total body fat as well as visceral fat and subcutaneous fat in the torso. In addition, participants had knee x-rays, rated severity of their knee pain and identified sites of joint pain on a body homunculus at the baseline, 30 month, and 60 month study visits. The association between the size of the fat depots with structural outcomes from baseline through 60 months (incident x-ray OA, MRI cartilage loss and worsening synovitis scores) and with pain outcomes over the same period (worsening pain; widespread pain and the number of painful joint sites) was assessed. We tested the association of sex specific quintiles of fat depot size with OA and pain outcomes performing regression analysis adjusted for age, sex, race, education, smoking, physical activity and BMI. For pain outcomes, we also adjusted for depressive symptoms and for all outcomes, adjusted for baseline status of the outcome (e.g. for WOMAC pain change, we adjusted for WOMAC pain at baseline).
Results: We studied 2,961 participants, of whom, 60.7% were women, mean age was 62.5 years and BMI 30.5 kg/m2. After adjustment for covariates including BMI, we found no association of any fat depot size with incident x-ray OA, cartilage loss or worsening synovitis on MRI (see figures below). On the other hand, total body fat and visceral fat deposit size were associated with worsening knee pain. Visceral fat in addition was associated with the number of painful joints and similar results were seen in the analyses of incident widespread pain. Subcutaneous fat was not associated with any of these pain measures. In these analyses, fat depots were associated with OA outcomes before analytic adjustment for BMI but positive results for only pain outcomes persisted after BMI adjustment.
Conclusion:
Visceral fat and total body fat are associated with increased musculoskeletal pain. We found no relationship between body fat and structural changes in OA. Further investigation into identification of specific inflammatory markers produced by body visceral fat may provide further insight into these findings.
To cite this abstract in AMA style:
Li S, Desai N, Neogi T, Schwartz A, Michael L, Wang N, Sun X, Nevitt M, Lewis B, Guermazi A, Roemer F, Segal N, Felson D. Visceral Fat Deposition Associated with Pain in Osteoarthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/visceral-fat-deposition-associated-with-pain-in-osteoarthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/visceral-fat-deposition-associated-with-pain-in-osteoarthritis/