Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Vasculitis is rare manifestation of systemic lupus erythematous (SLE) that often leads to increased morbidity and mortality. Vasculitis prevalence in SLE patients have ranged from 11-36% and can be mild to life-threatening. While there have been limited studies focusing on cutaneous small vessel vasculitis, there are not many studies focusing on risk factors of patients that develop vasculitis within a large longitudinal SLE cohort. The purpose of our study is to identify SLE clinical characteristics associated with vasculitis, testing the hypothesis that certain organ involvement with SLE will be associated with a higher risk of vasculitis.
Methods: We collected data from consented patients within our institutional longitudinal SLE Database. Data included sex, race, ethnicity, age at lupus onset, SLE classification criteria, medical history, and complications in patients’ disease course, including history of vasculitis. If history of vasculitis was present, notes from the database visits and electronic medical record encounters were reviewed to determine what type of vasculitis was present and which organ systems were involved. Once form of vasculitis and organ involvement was confirmed, Stata v15 was utilized to perform descriptive statistics, Chi-squared, Fisher’s exact, and t-tests, as appropriate.
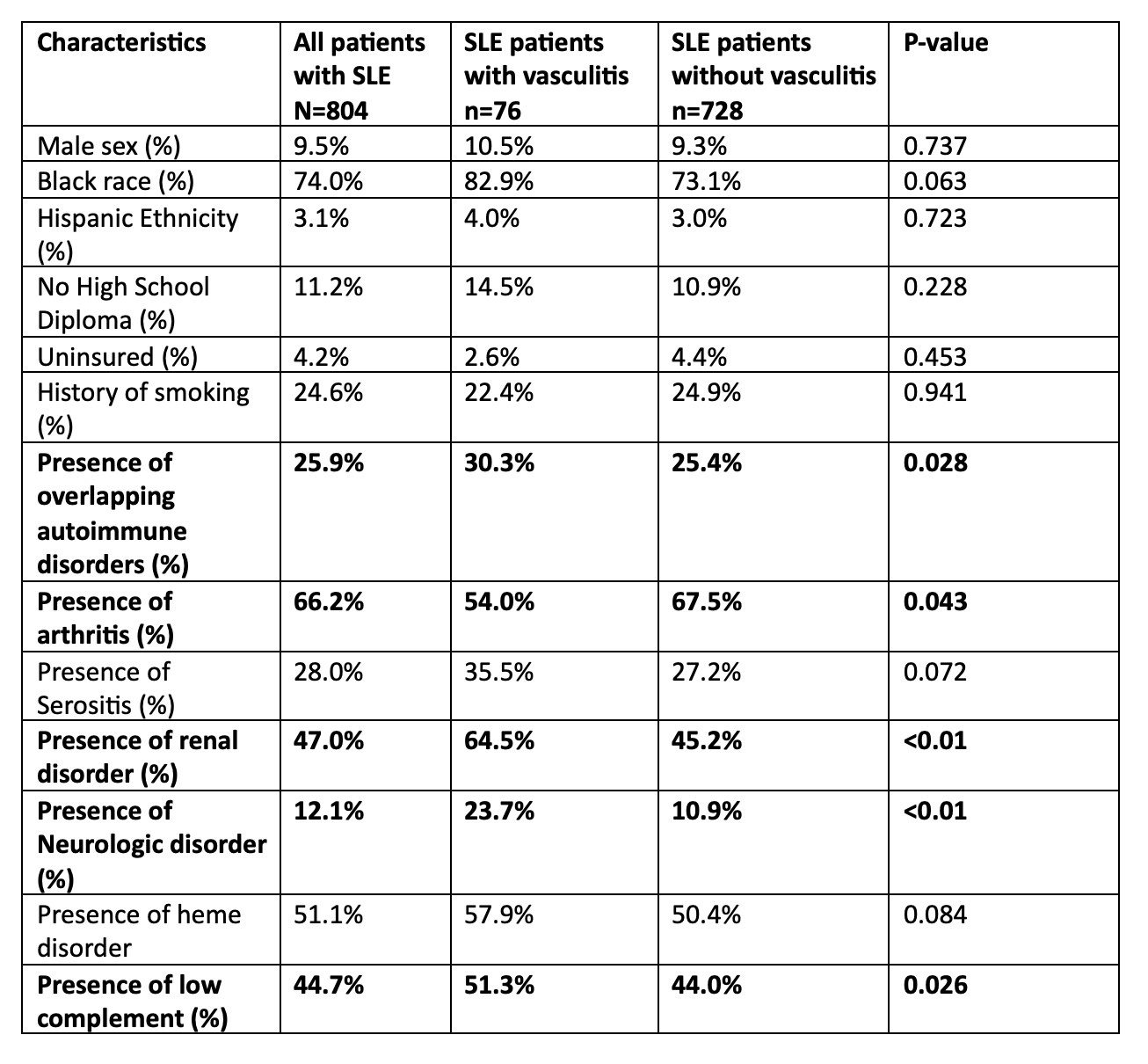
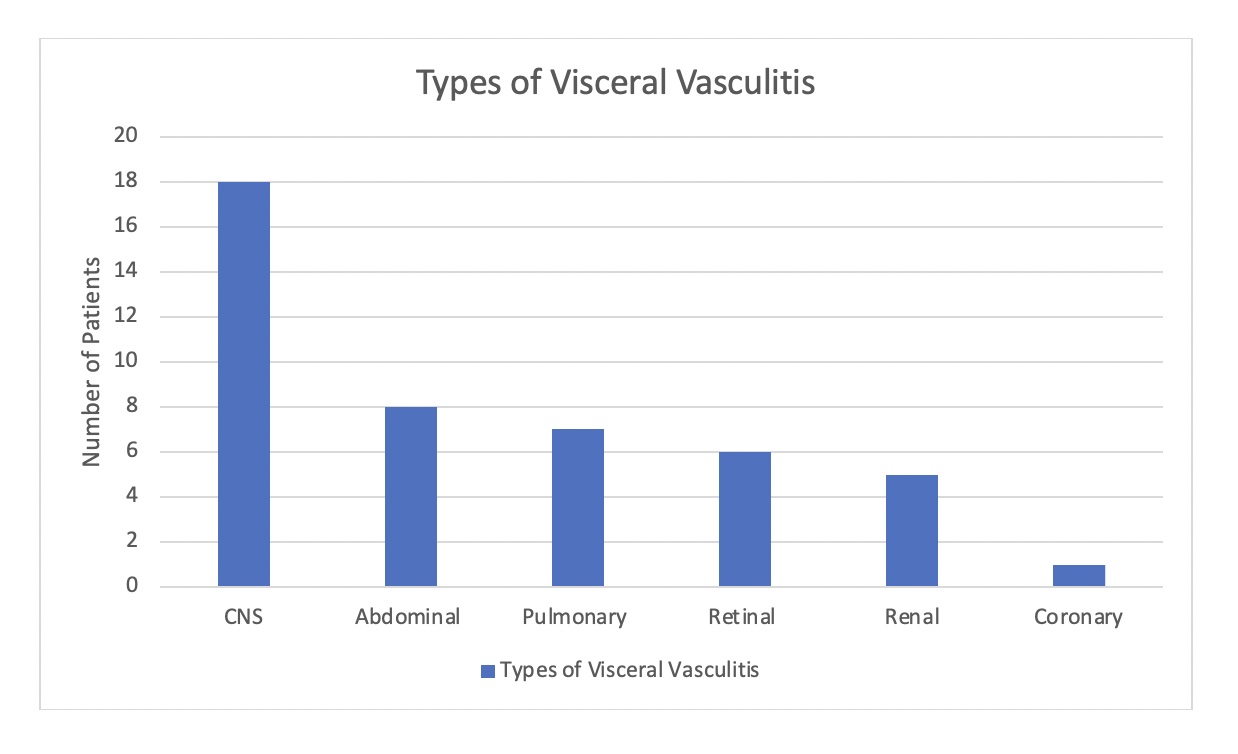
Results: Of the 804 patients with SLE included our study, 728 (90.5%) were female, 595 (74%) were Black, and 76 (9.5%) had a history of vasculitis (Table 1). 44.7% had visceral vasculitis, 43.4% had cutaneous vasculitis, 7.9% had both cutaneous and visceral vasculitis. Out of the 40 patients that had visceral vasculitis, the breakdown of specific organ involvement was noted (Figure 1). Overall, most of patients with vasculitis had CNS, abdominal, or pulmonary involvement. The mean age of SLE onset in patients with vasculitis was 27.3 ± 13.0, compared to 31.5 ± 14.0 in patients without vasculitis. We analyzed the correlation between vasculitis and many factors, including race, ethnicity, symptoms such as arthritis and serositis, smoking history, and others (Table 1). We found that presence of other autoimmune disorders, history of renal disorder, and history of neurologic disorder, and low complement was associated with the development of vasculitis. Although mortality rates were higher among patients with vasculitis (21.1% vs 14.0%, p=0.099), the difference was not statistically significant.
Conclusion: Among patients with SLE from a unique population-based cohort, vasculitis was a less common (9.5%) manifestation, yet with important implications for SLE severity and organ involvement. Given the low prevalence of vasculitis, we were limited in ability to identify rare associations, however the strong negative association with arthritis adds to what was previously described in the literature. Based on our findings, presence of low complement, renal, and/or neurologic disorder among patients with SLE could be important clues to the identification of early vasculitis, prompting recognition and treatment which is crucial to improve outcomes.
To cite this abstract in AMA style:
Cosentino E, Blanchard M, Kamen D, Oates J. Vasculitis Associations Among Patients with Systemic Lupus Erythematous [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/vasculitis-associations-among-patients-with-systemic-lupus-erythematous/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/vasculitis-associations-among-patients-with-systemic-lupus-erythematous/