Session Information
Date: Monday, November 18, 2024
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders II
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: VEXAS (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic) syndrome is a recently defined clinical entity that causes hematologic and autoinflammatory symptoms. Since its initial description in 2020, it was recognized to mimic many other rheumatologic conditions. For example, in the incident VEXAS cohort of 25 patients described by Beck and colleagues, 60% had been diagnosed with relapsing polychondritis, 12% with polyarteritis nodosa, and 4% with giant cell arteritis (1). Our objective is to define the prevalence, distribution, and characteristics of vasculitis in a cohort of patients with VEXAS syndrome.
Methods: Patients with VEXAS syndrome, verified by positive UBA1 mutation, were included. Chart review was performed to identify patient characteristics and outcomes. Vasculitis diagnosis was based on either histopathology showing vascular inflammation or non-invasive angiography findings. Summary statistics were calculated.
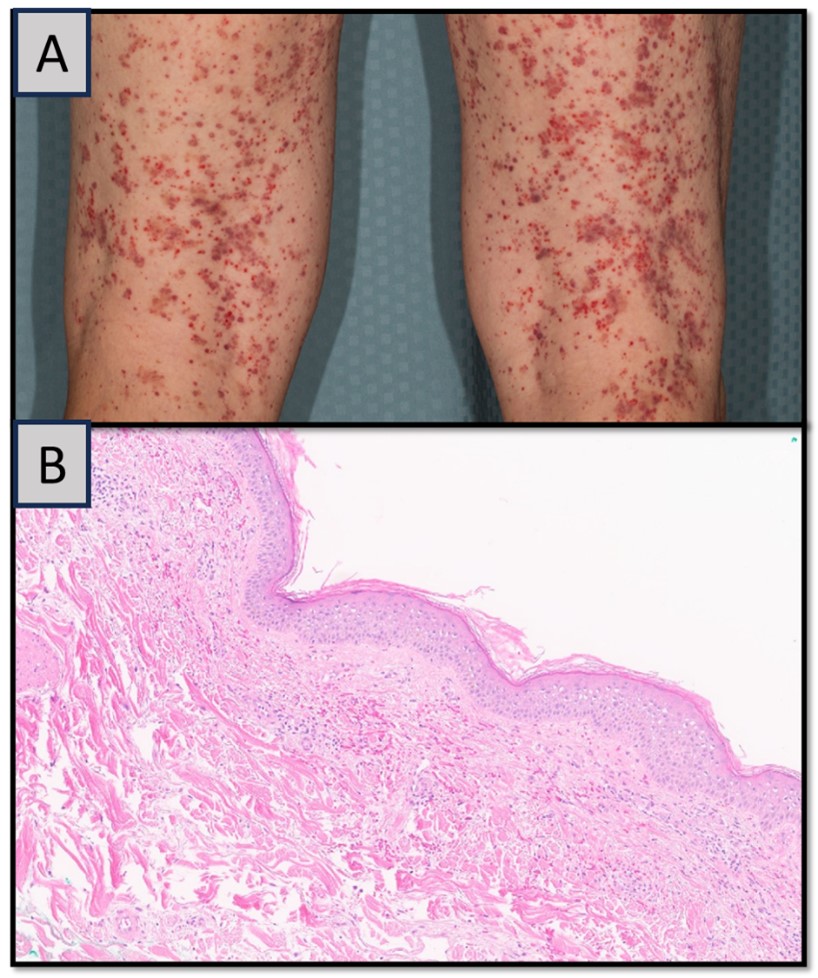
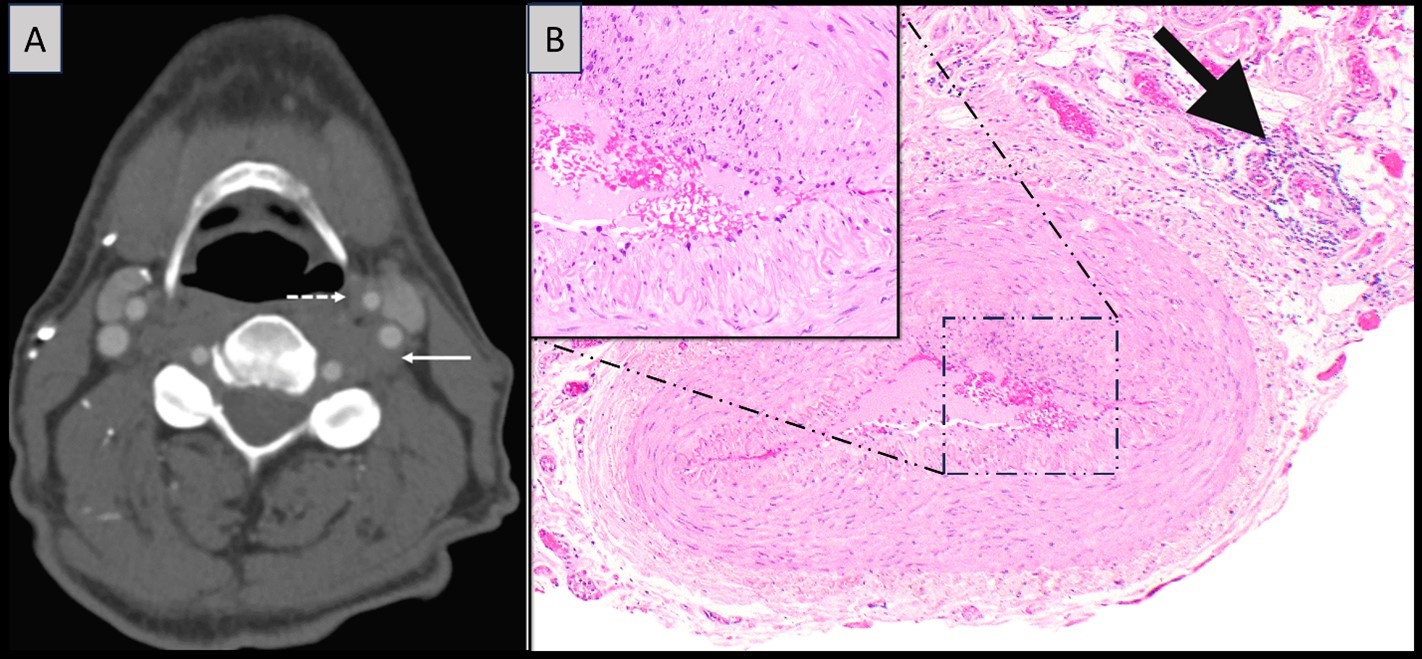
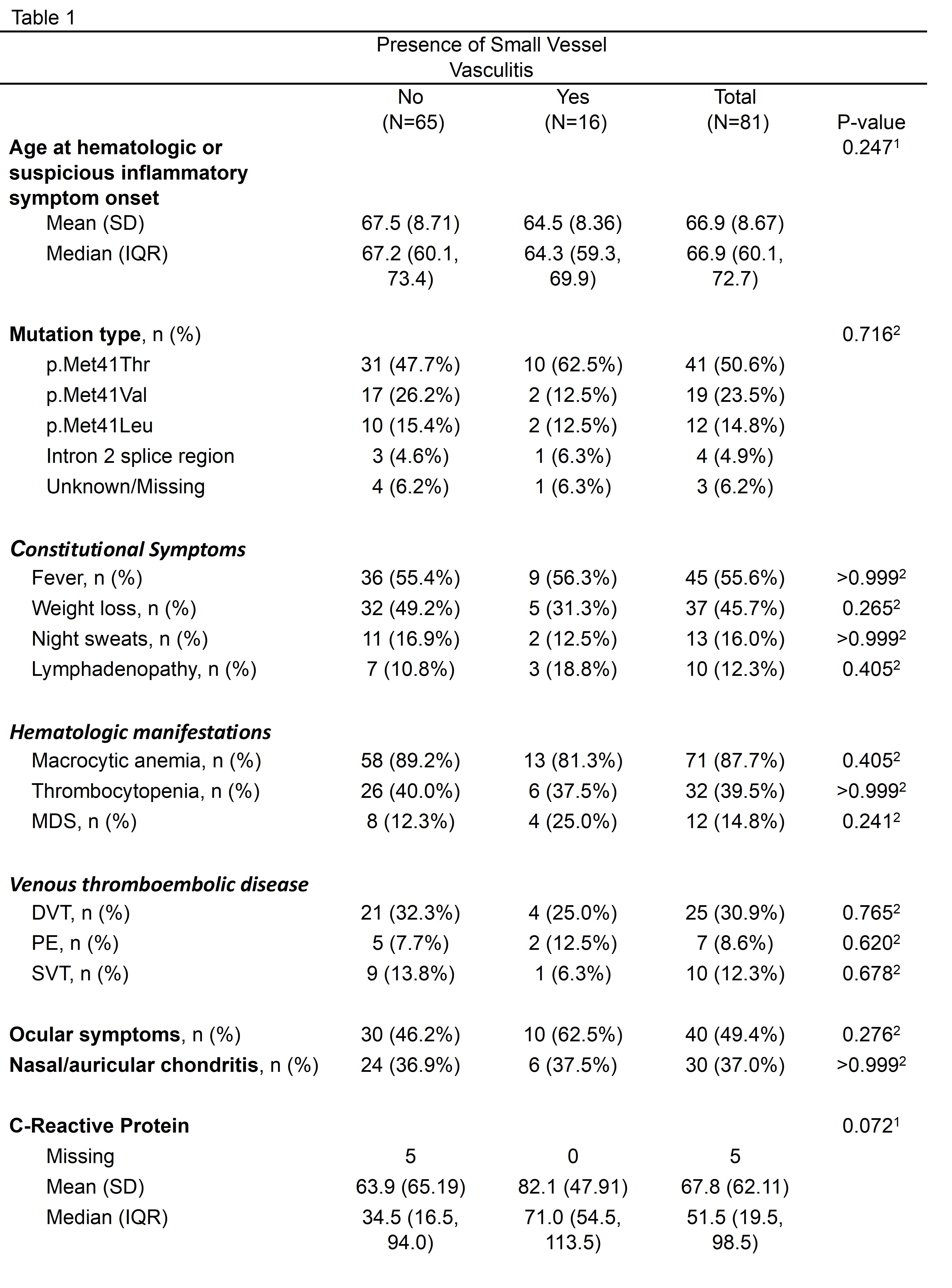
Results: Eighty-one patients met inclusion criteria. All were male with a median age of onset of 66.9 years (IQR 60.1, 72.7). Median (IQR) follow up was 4.0 (2.2-5.4) years during which 22 patients (27.2%) had histopathology or non-invasive angiography positive for vascular inflammation. Vasculitis subtypes included cutaneous small vessel vasculitis (16/81 19.8%), ANCA-associated vasculitis (2.5%), cutaneous medium vessel vasculitis (2.5%), and large vessel vasculitis (2.5%). No patient had more than one vessel size involved. Histopathology in small vessel vasculitis patients was consistent with cutaneous leukocytoclastic vasculitis in the majority (Figure 1). One patient had leukocytoclastic peritubular capillaritis on renal biopsy. Cranial symptoms (headache, vision changes, or jaw pain) were noted in 16 (19.8%). Two patients exhibited large vessel involvement with confirmed carotid thickening on non-invasive angiography; one of these had a positive temporal artery biopsy revealing an unusual pattern of focal endothelialitis consisting of mixed inflammatory infiltrate and neutrophils (Figure 2). Disease characteristics did not differ between those with cutaneous small vessel vasculitis to those without (Table 1).
Conclusion: VEXAS syndrome manifests as a variable vessel vasculitis in a quarter of patients, with cutaneous small and medium vessel involvement being particularly common. Some patients may have positive ANCA serologies or even renal leukocytoclastic vasculitis leading to misdiagnosis. Cranial symptoms are common and may mimic giant cell arteritis, though documented large vessel inflammation is rare.
To cite this abstract in AMA style:
Sullivan M, Kalantari K, Mead-Harvey C, Kusne Y, Patnaik M, Mangaonkar A, Go R, Montes D, Reichard K, Olteanu H, Bois M, Hines A, Sartori-Valinotti J, Warrington K, Koster M. Vasculitis Associated with VEXAS Syndrome [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/vasculitis-associated-with-vexas-syndrome/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/vasculitis-associated-with-vexas-syndrome/