Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Eosinophilic Granulomatosis with Polyangiitis (EGPA) is a rare systemic vasculitis that can lead to significant morbidity and mortality. This study aims to evaluate the demographic, clinical, and hospital-related characteristics associated with in-hospital mortality among EGPA hospitalizations using a claims-based US national database.
Methods: A retrospective analysis of the National Inpatient Sample (NIS) database from 2017 – 2021 was conducted to identify adult hospitalizations with a primary or secondary diagnosis of EGPA (ICD 10: M30.1). Descriptive statistics were used to compare patients discharged alive and those who suffered in-hospital mortality. All variables with p ≤ 0.2 in the univariable screen were included in a multivariable logistic regression model to assess independent predictors of in-hospital death. p ≤ 0.05 was considered significant in multivariable analysis. Cells of data containing hospitalization records with a value of 1 to 10 were not reported to protect hospital privacy as per the Healthcare Cost and Utilization Project (HCUP) data service agreement.
Results: A total of 9,095 hospitalizations for EGPA were identified, with an in-hospital mortality rate of 2.9% (n = 265) (Table 1). Patients who died in-hospital were older (median age 69 vs. 63 years ; p = 0.018), had a higher median Charlson Comorbidity Index (CCI) (3 vs. 2; p = 0.01), higher acute kidney injury (AKI) (66.0% vs. 19.9%; p < 0.001), higher alveolar hemorrhage (5.7% vs. 0.8%; p < 0.001), higher concurrent infection (79.2% vs. 46.2%; p < 0.001), higher heart failure (37.7% vs. 22.9%; p = 0.012), longer median hospital length of stay (10 vs. 4 days; p < 0.001), and higher median total hospital charges ($154,087 vs. $43,916; p < 0.001). The variables from the univariable screen showing an association with in-hospital mortality were age, male sex, Medicare insurance, Medicaid insurance, private insurance, CCI, AKI, alveolar hemorrhage, heart failure, hemophagocytic lymphohistiocytosis, infection, and myocardial infarction (Table 2).In multivariable regression analysis, independent predictors of in-hospital mortality included AKI (OR 4.81; 95% CI 2.50 - 9.25), alveolar hemorrhage (OR 6.92; 95% CI 1.47 - 32.46), and infection (OR 3.56; 95% CI 1.81 - 7.01) (Table 3). Age, sex, insurance type, and comorbidity burden were not independent predictors of in-hospital death in EGPA.
Conclusion: In this large, nationally representative cohort, EGPA hospitalizations had a 2.9% in-hospital mortality rate. AKI, alveolar hemorrhage, and infection were strong independent predictors of mortality. These findings highlight the need for early recognition and management of these complications to improve outcomes in hospitalized EGPA patients.
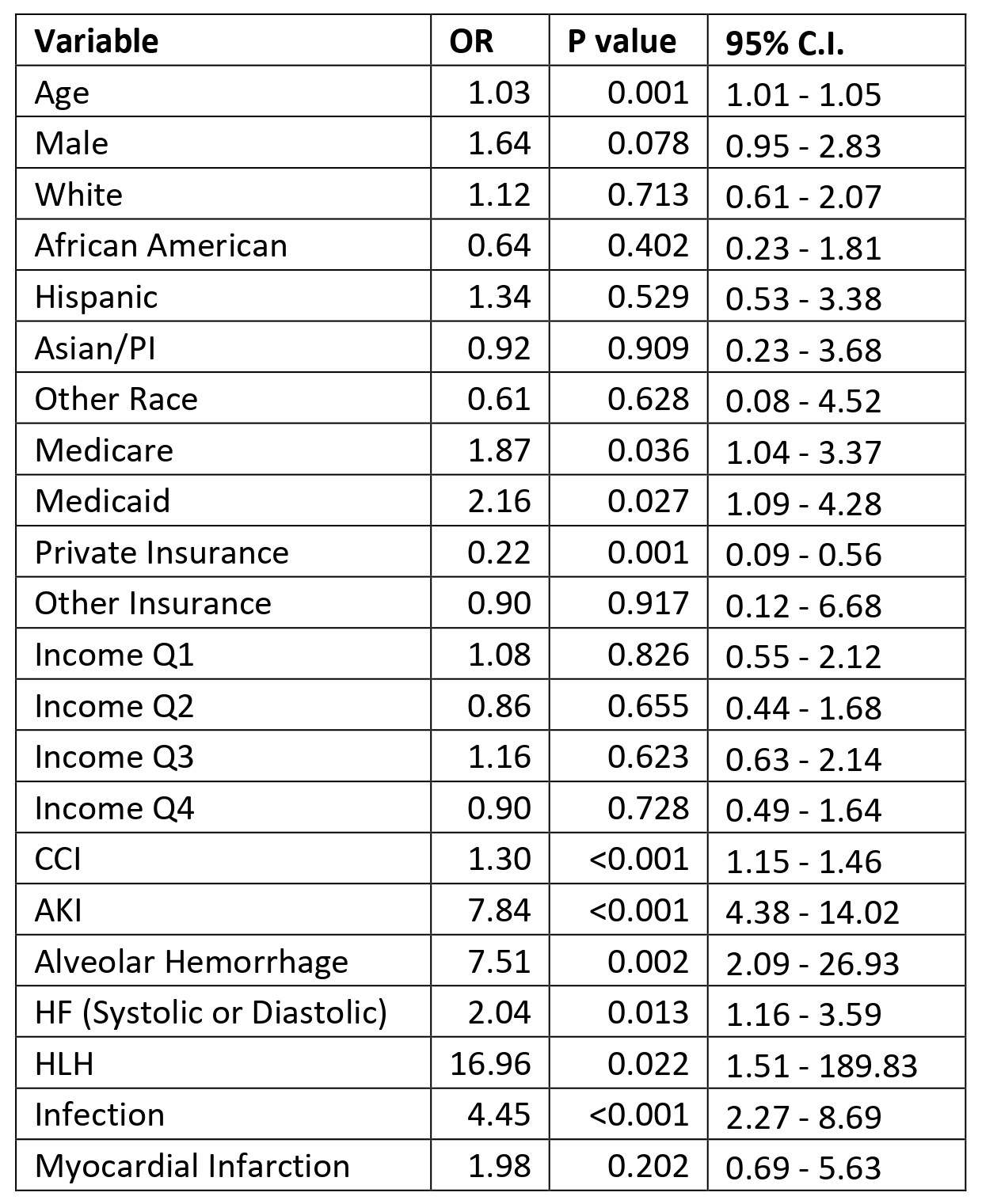 Table 1: Descriptive Characteristics of Adult Hospitalizations with EGPA from the National Inpatient Sample Database 2017-2021 (n=9,095).
Table 1: Descriptive Characteristics of Adult Hospitalizations with EGPA from the National Inpatient Sample Database 2017-2021 (n=9,095).
Abbreviations: AKI= Acute Kidney Injury; CCI= Charlson Comorbidity Index; EGPA=Eosinophilic Granulomatosis with Polyangiitis; HLH= Hemophagocytic Lymphohistiocytosis; HF= Heart Failure; IQR=interquartile range; LOS=Length of Stay; n=number; NIS= National Inpatient Sample Database; NR = not reported as below permitted reporting threshold (≤10 cases); PI=Pacific Islander.
.jpg) Table 2: Univariable Logistic Regression for In-hospital Death for EGPA from NIS 2017-2021.
Table 2: Univariable Logistic Regression for In-hospital Death for EGPA from NIS 2017-2021.
Abbreviations: AKI= Acute Kidney Injury; CCI= Charlson Comorbidity Index; EGPA=Eosinophilic Granulomatosis with Polyangiitis; HLH= Hemophagocytic Lymphohistiocytosis; HF= Heart Failure; NIS= National Inpatient Sample Database.
*Univariable analysis was not conducted for Native American, Self Pay, No Charge and Myocarditis as there were no observed deaths in that category.
.jpg) Table 3: Multivariable Logistic Regression for In-hospital Death for EGPA from NIS 2017-2021.
Table 3: Multivariable Logistic Regression for In-hospital Death for EGPA from NIS 2017-2021.
Abbreviations: AKI= Acute Kidney Injury; CCI= Charlson Comorbidity Index; EGPA= Eosinophilic Granulomatosis with Polyangiitis; HLH= Hemophagocytic Lymphohistiocytosis; HF= Heart Failure; NIS= National Inpatient Sample Database;
To cite this abstract in AMA style:
Natu A, Small I, Arora S, Manadan A. Variables Associated with In-Hospital Mortality in Adult Eosinophilic Granulomatosis with Polyangiitis from the National Inpatient Sample Database 2017-2021 [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/variables-associated-with-in-hospital-mortality-in-adult-eosinophilic-granulomatosis-with-polyangiitis-from-the-national-inpatient-sample-database-2017-2021/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/variables-associated-with-in-hospital-mortality-in-adult-eosinophilic-granulomatosis-with-polyangiitis-from-the-national-inpatient-sample-database-2017-2021/
