Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Valuable information on cardiovascular disease outcomes can be obtained from large cohort studies. Such studies often rely on self-reported events, which are best validated with linkage to administrative data or review of electronic medical records. Given the increased risk of cardiovascular disease in patients with inflammatory rheumatic diseases, we aimed to assess the validity of patient-reported and physician-recorded cardiovascular events in a large cohort of patients with psoriatic disease.
Methods: Patients enrolled in a prospective cohort study from 1978 to 2018 were included in the analysis. Participants are assessed by a rheumatologist at 6-12 month intervals according to a standardized protocol that includes information about co-morbidities. Typically, patients report their co-morbidities which are recorded by the physician. The information is stored in a computerized database. We searched the database for records of cardiovascular events recorded during the follow-up period. Cardiovascular outcomes included angina, myocardial infarction (MI), revascularization procedures, congestive heart failure (CHF), cerebrovascular accident (CVA) and transient ischemic attack (TIA). The accuracy of the outcomes was verified by linkage to hospital discharge databases and review of medical records, which was considered as the gold standard ascertainment method. The validity of cardiovascular events by rheumatologists was assessed by calculating sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV).
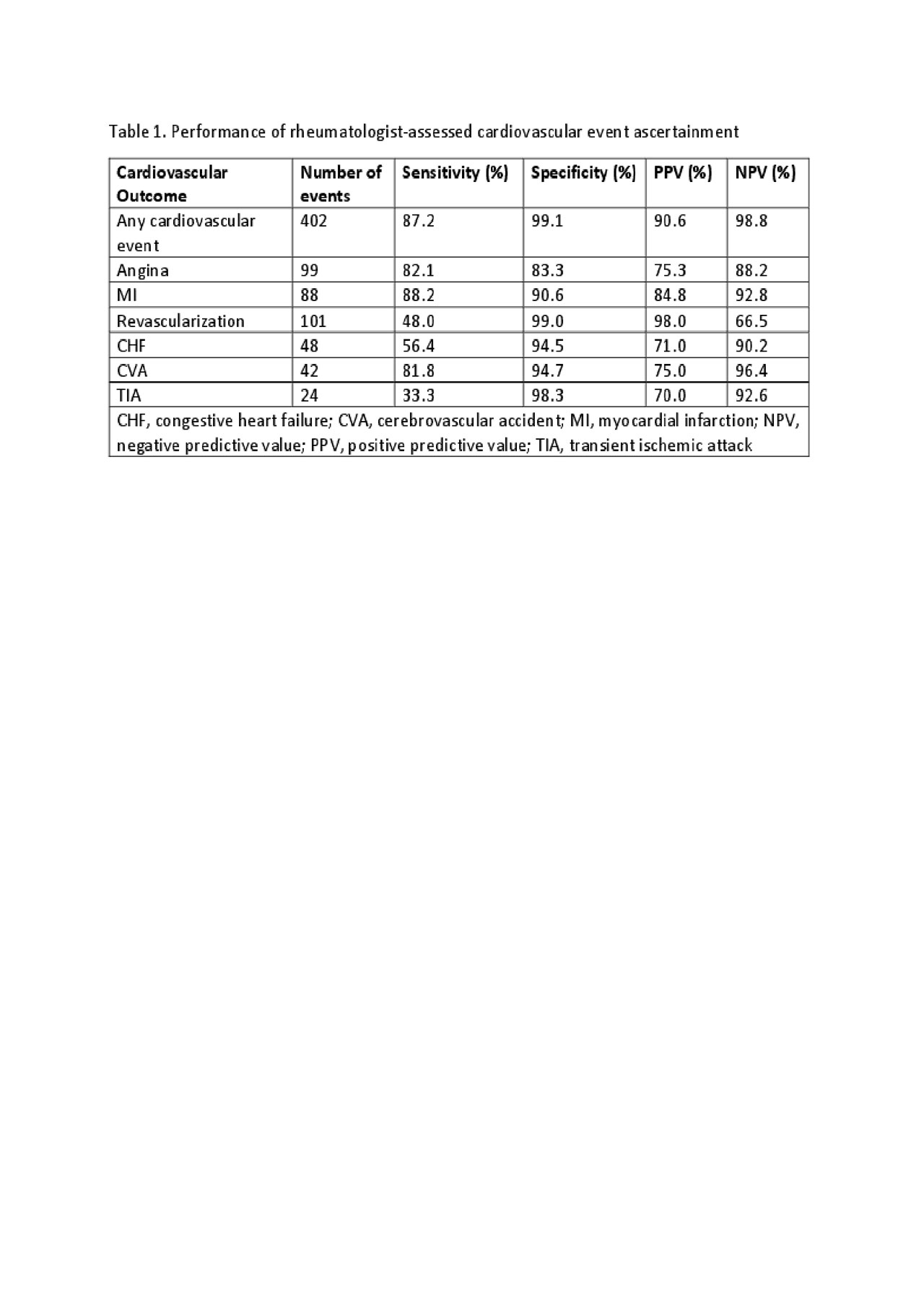
Results: 2,171 patients with psoriatic disease (1498 with psoriatic arthritis, 673 with psoriasis only) were followed in the cohort from 1978 to 2018. The mean duration of follow-up for patients with psoriatic arthritis and psoriasis only was 10.2 years and 4.1 years, respectively. During this period, 204 (9.4%) patients reported 402 events (Table 1). Sixty-three events from the lost-to-follow up period were excluded. Overall the accuracy of patient-reported cardiovascular events was good to excellent. The sensitivity, specificity, PPV, NPV for any cardiovascular event was 87%, 99%, 91%, 99%, respectively. A similar pattern of results was observed for angina, MI and CVA. Identification of TIA showed poor sensitivity (33%), followed by revascularization (48%) and CHF (56%). NPV of all outcomes were excellent, with the exception of revascularization.
Conclusion: Ascertainment of self-reported cardiovascular events by rheumatologists is fairly accurate for identifying incident occurrences of cardiovascular events. Additional methods, such as record linkage and chart review, could be used to identify events not captured by conventional methods.
To cite this abstract in AMA style:
Colaco K, Chandran V, Gladman D, Eder L. Validity of Patient-reported Cardiovascular Events in a Large Longitudinal Cohort of Patients with Psoriatic Arthritis and Psoriasis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/validity-of-patient-reported-cardiovascular-events-in-a-large-longitudinal-cohort-of-patients-with-psoriatic-arthritis-and-psoriasis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/validity-of-patient-reported-cardiovascular-events-in-a-large-longitudinal-cohort-of-patients-with-psoriatic-arthritis-and-psoriasis/