Session Information
Session Type: Poster Session A
Session Time: 6:00PM-7:00PM
Background/Purpose: Chronic nonbacterial osteomyelitis (CNO) is an aseptic autoinflammatory bone disease of unknown etiology. This diagnosis can be delayed due to the non-specific nature of symptoms, referral patterns to non-rheumatology specialists and normal imaging studies. New classification criteria have been proposed for CNO and were presented at the American College of Rheumatology scientific meeting in 2022. This study seeks to validate these new classification criteria.
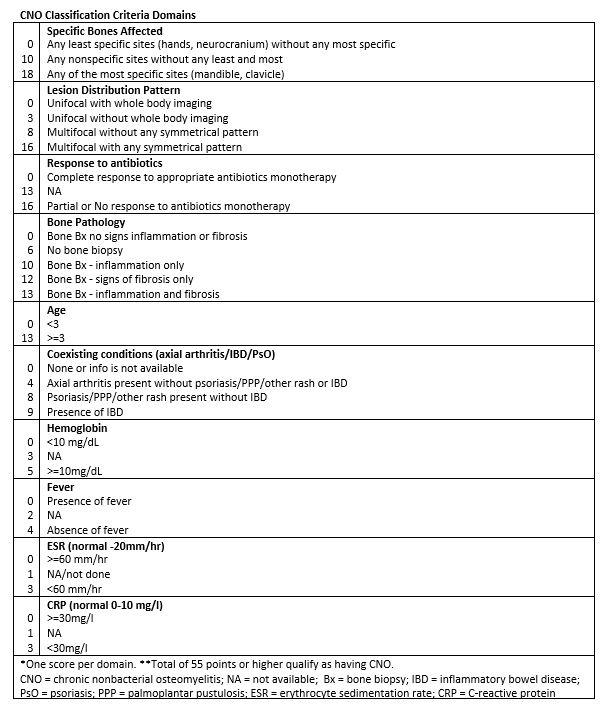
Methods: This is a retrospective case-series of pediatric patients diagnosed with CNO (n=34). They were diagnosed and managed between 2012 and 2022 at the University of Virginia in Charlottesville, Virginia and Bon Secours Mercy Health in Richmond, Virginia. The entry criteria of chronic bone pain, age 18 years, abnormal radiograph and/or MRI were used prior to applying the newly proposed classification criteria. Tendomains were evaluated to indicate whether a patient has CNO; those who scored 55 points or higher qualified (see table). The clinical manifestations, laboratory results, and imaging studies that lead to a diagnosis of CNO were reviewed in detail. We applied and validated the newly proposed classification criteria for CNO to this Virginia cohort of previously diagnosed pediatric CNO patients. We also reviewed the characteristics of those that did not fulfill this classification criteria.
Results: Upon application of the newly proposed classification criteria for CNO, 31 out of 34 patients (91%) were found to meet this classification criteria. Of those that did not fulfill the criteria but carry the diagnosis of CNO (n=3) none had “least specific sites” such as hands orneurocranium, all had elevated ESR and two out of three had an initial response to antibiotics. Their scores were 49, 51 and 53 with classification criteria being met with 55 or higher. The average age of diagnosis was 10 (range 2-17) years-old with the average time between onset of symptoms to confirmed radiographic evidence being 25 (range 1-120) months. The most common presenting symptoms were bone pain (100 %) and arthritis (52%) with fever (23%) and rash (3%) being less common. Elevated ESR (39%) and CRP (39%) were found at initial visit with rheumatology. Evidence of commonly seen radiographic abnormalities leading to CNO diagnosis was found with regional MRI (65%), bone scan (42%) with some requiring full body MRI (26%) to confirm other lesions. Some patients did have multiple imaging studies including X-ray, CT, bone scan, MRI and bone biopsy in their workup.
Conclusion: This retrospective chart review validates the newly proposed classification criteria for CNO. We conclude that these criteria are easy to apply even in the absence of a bone biopsy or advanced imaging studies. This will aid in the development of a homogeneous cohort for future studies in CNO.
To cite this abstract in AMA style:
Lee K, Kim A, Patel A. Validation of Newly Proposed Classification Criteria for Pediatric Chronic Nonbacterial Osteomyelitis: A Virginia Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/validation-of-newly-proposed-classification-criteria-for-pediatric-chronic-nonbacterial-osteomyelitis-a-virginia-cohort/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/validation-of-newly-proposed-classification-criteria-for-pediatric-chronic-nonbacterial-osteomyelitis-a-virginia-cohort/