Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) has a complex and poorly understood etiology and is difficult to diagnose due to its varied presentation across many organ systems. While we know genetic factors and environmental exposures contribute to SLE development, there is still much variability not explained by genetics or exposures. Socioeconomic factors such as race have also been shown to affect the prevalence of SLE. We aim to evaluate measures of social determinants of health (SDOH) and environmental factors that contribute to the risk of SLE symptomatology.
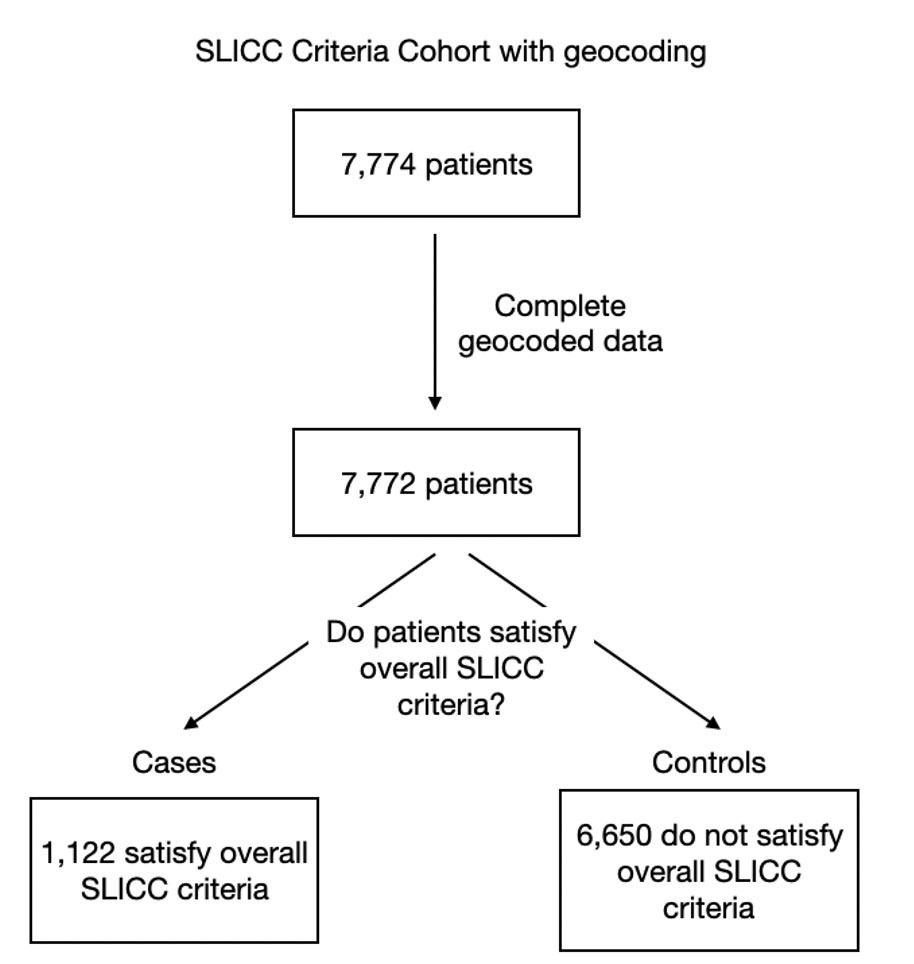
Methods: Electronic medical record (EMR) data were derived from select sites participating in a large NIH-funded multisite consortium; these data included demographic and clinical data elements spanning 2000-2020. Geocoding to the level of census tracts was completed in 2015 using patients’ latest address. Our cohort consisted of all consortium subjects with geocoded addresses. Cases were defined as patients who satisfied the overall SLICC classification criteria on clinical data from the EMR. Controls were patients who did not satisfy the overall SLICC criteria (Figure 1). From geocoded addresses, we imputed the urban or rural status of the patients as a proxy for social and environmental stressors. Race was self-reported and grouped into White, Black or African American, and Other Non-White. Deprivation was measured by area deprivation index (ADI) that ranged from 0 to 1, with 1 being highest deprivation.1 We used a multivariate logistic regression model to determine if an individual’s neighborhood urbanicity, race, and neighborhood deprivation are associated with meeting the overall SLICC criteria, correcting for age, sex, and distance from the hospital.
- Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population-based cohort study. Ann Epidemiol. 2019;30:37-43.
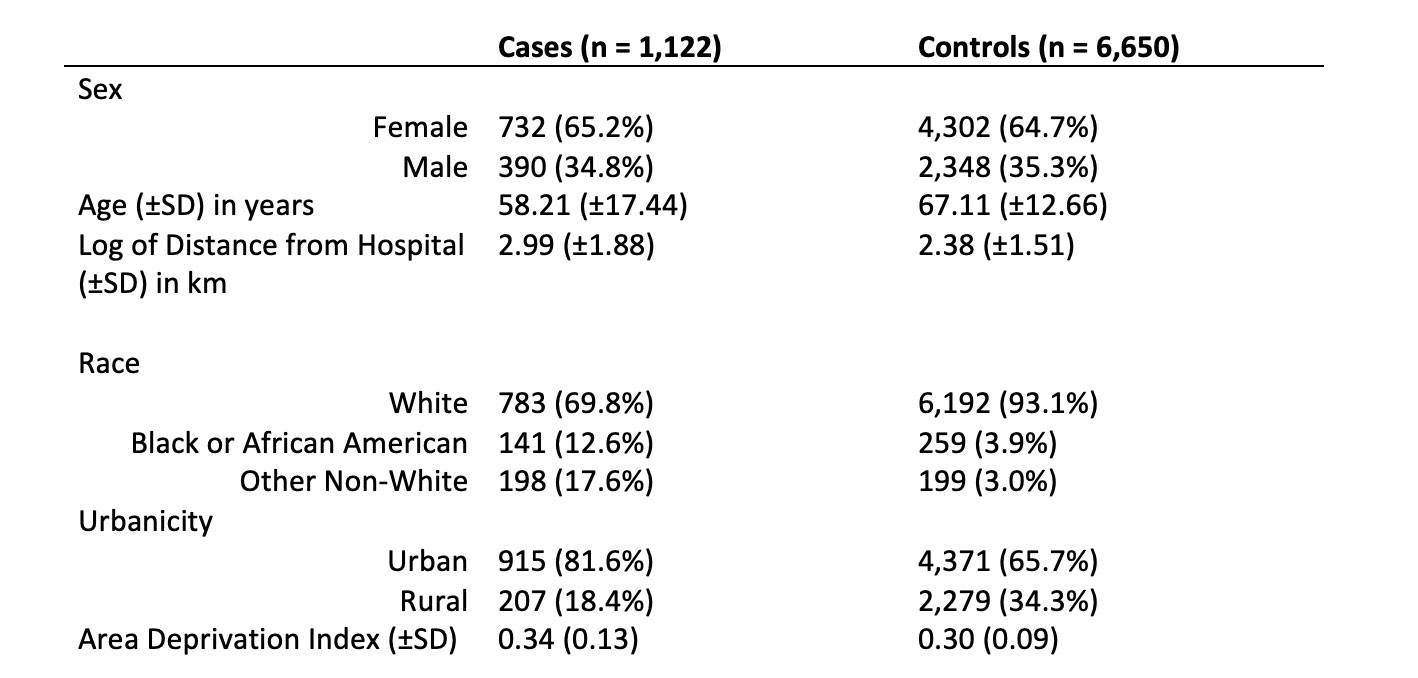
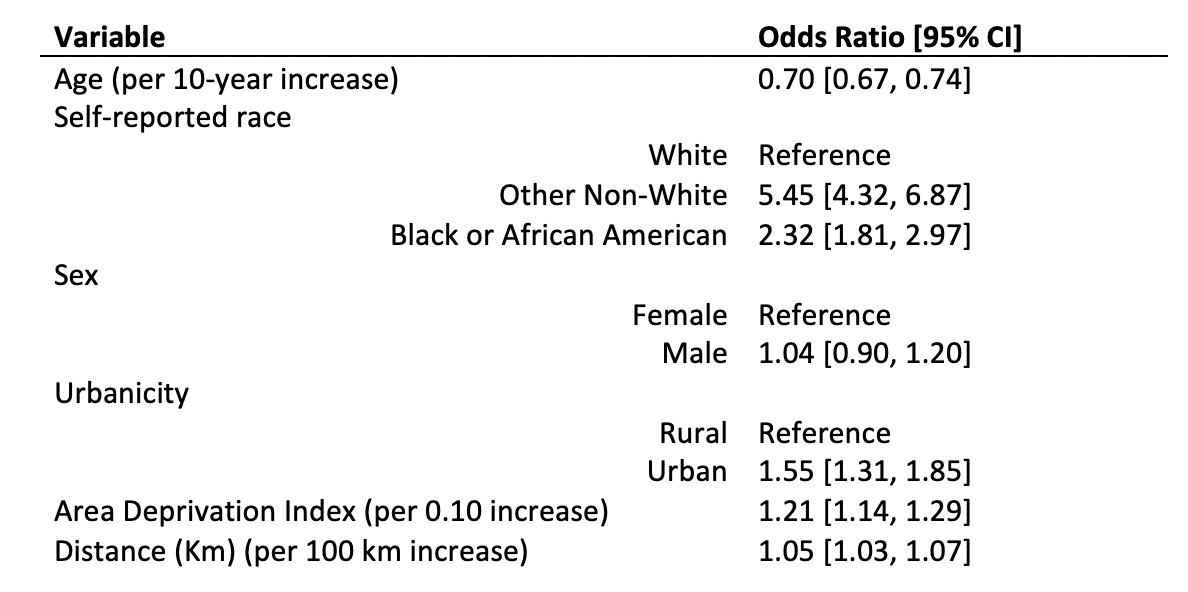
Results: In our cohort 1,122 people met the overall SLICC criteria (cases) for SLE whereas 6,650 did not (controls) (Table 1). Residential distance from the hospital was skewed (skewness 8.17) due to the hospital catchment areas. Every 100 km increase in distance was associated with a 1.05 increased odds of meeting SLICC criteria (95% CI: [1.03, 1.07]). We found that patients living in an urban census tract relative to patients in rural census tracts (OR: 1.55; 95% CI: [1.31, 1.85]) and greater ADI (OR: 1.21 per 0.10 unit increase in index; 95% CI: [1.14, 1.29]) were associated with increased odds of meeting the overall SLICC criteria relative to a rural census tract. Black or African American race was associated with an increase in odds (OR: 2.32; 95% CI: [1.81, 2.97]) and Other Non-White patients had an even greater odds of satisfying the SLICC criteria (OR: 5.45; 95% CI: [4.32, 6.87]) compared to White patients (Table 2).
Conclusion: We highlight the importance of measures of SDOH in SLE symptom presentation. Further investigation into social stressors has the potential to improve understanding of SLE symptom etiology.
To cite this abstract in AMA style:
Song J, Forrest N, Mittendorf K, Wei W, Kottyan L, Ramsey-Goldman R, Walunas T, Kho A. Utilization of Electronic Health Record Data to Evaluate the Impact of Urban Environment on Risk of Systemic Lupus Erythematosus Symptoms [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/utilization-of-electronic-health-record-data-to-evaluate-the-impact-of-urban-environment-on-risk-of-systemic-lupus-erythematosus-symptoms/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/utilization-of-electronic-health-record-data-to-evaluate-the-impact-of-urban-environment-on-risk-of-systemic-lupus-erythematosus-symptoms/