Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Because systemic lupus erythematosus (SLE) is a complex and heterogeneous disease, we have developed a conceptual model that divides SLE activity into two dimensions: Type 1 SLE consists of inflammatory activity, including arthritis, nephritis, and rashes; Type 2 SLE includes fatigue, myalgia, mood disturbance, and cognitive dysfunction. We theorize that different treatment paradigms may be needed for each dimension because of differences in underlying pathogenesis. In this study, we assessed whether distinct patterns of patient-reported symptoms could provide meaningfully distinguish between Type 1 and Type 2 SLE activity.
Methods: Consecutive SLE patients meeting SLICC criteria in a university lupus clinic registry completed two questionnaires: the Systemic Lupus Activity Questionnaire (SLAQ) and the ACR Fibromyalgia Severity Score (FSS). SLEDAI and physician global assessment (PGA; 0-3) were also recorded. High Type 1 SLE activity was defined as SLEDAI ≥4 (scored without labs), SLEDAI ≥6, active nephritis, or PGA ≥1.5. High Type 2 SLE activity was defined as FSS ≥8. Patients with both high Type 1 and 2 activity were defined as Mixed SLE, and patients with low Type 1 and 2 activity were defined as Minimal SLE.
Latent class analysis (LCA) was used to identify classes of SLE patients based on SLAQ symptoms (muscle pain, stiff joint, malar rash, alopecia, oral or nasal ulcers, chest pain with a deep breath, depression, and a patient global assessment of disease activity) and FSS symptoms (fatigue, cognitive dysfunction, waking unrefreshed, and total areas of widespread pain). Latent classifications were then compared to the clinically defined Type 1 and 2 SLE classification groups to determine if the PRO-derived classes could identify the Type 1/2 disease classifications.
Results: The study included 225 SLE patients. A 3-class solution provided the best fit of the data (entropy >0.90) and classified patients into low (n=85, 38%), medium (n=110, 49%), and high (n=40, 18%) PRO severity classes.
Patients in the low PRO severity class were primarily asymptomatic (Figure 1). While most patients were classified as Minimal SLE, 29% had Type 1 activity, half of whom had active nephritis (Figure 2).
The medium PRO severity class was characterized by mild-moderate fatigue (85%), stiff joints (84%), and waking unrefreshed (70%). Patients in this class were evenly distributed across the a priori-defined Type 1 and 2 SLE groups.
The high PRO severity class reported the most severe symptoms, including moderate-severe fatigue (100%), waking unrefreshed (95%), stiff joints (93%), muscle pain (92%), and cognitive dysfunction (65%), as well as high patient-global assessment scores (average: 7.3) and areas of widespread pain (average: 10.4). All patients in this class had active Type 2 SLE, with 33% having inactive and 68% having active Type 1 SLE.
Conclusion: While the LCA was able to classify SLE patients based on the severity of Type 2 SLE activity, this approach was unable to yield a class that was exclusive to Type 1 SLE activity. Ongoing research will explore whether including clinician-reported or laboratory data will better distinguish between these four SLE groups.
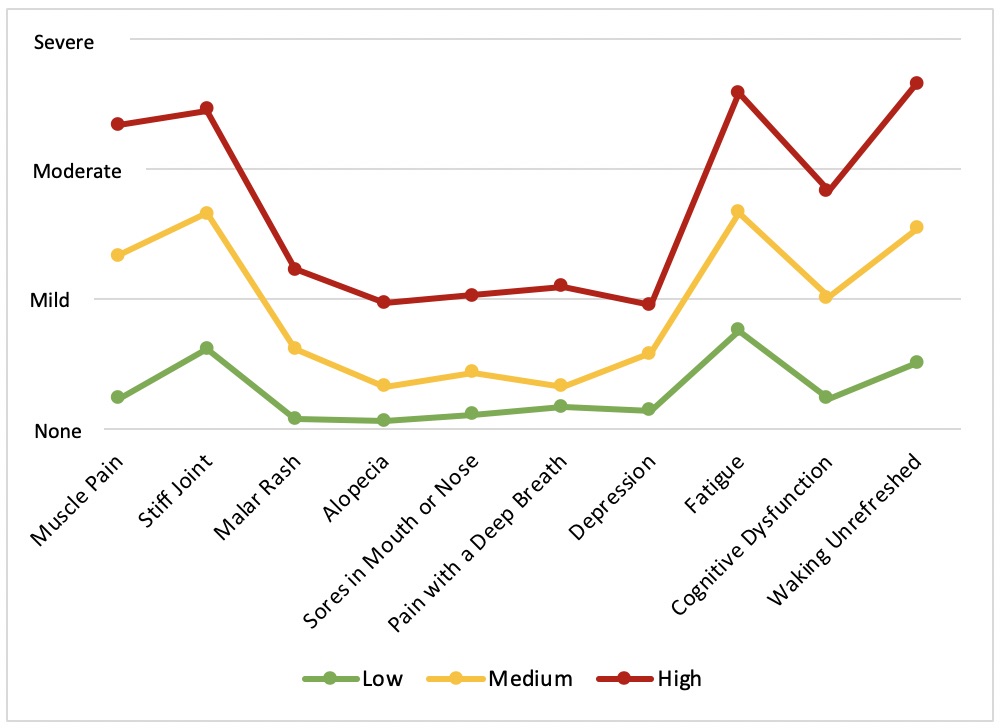 Figure 1. Average patient-reported symptoms by severity class.
Figure 1. Average patient-reported symptoms by severity class.
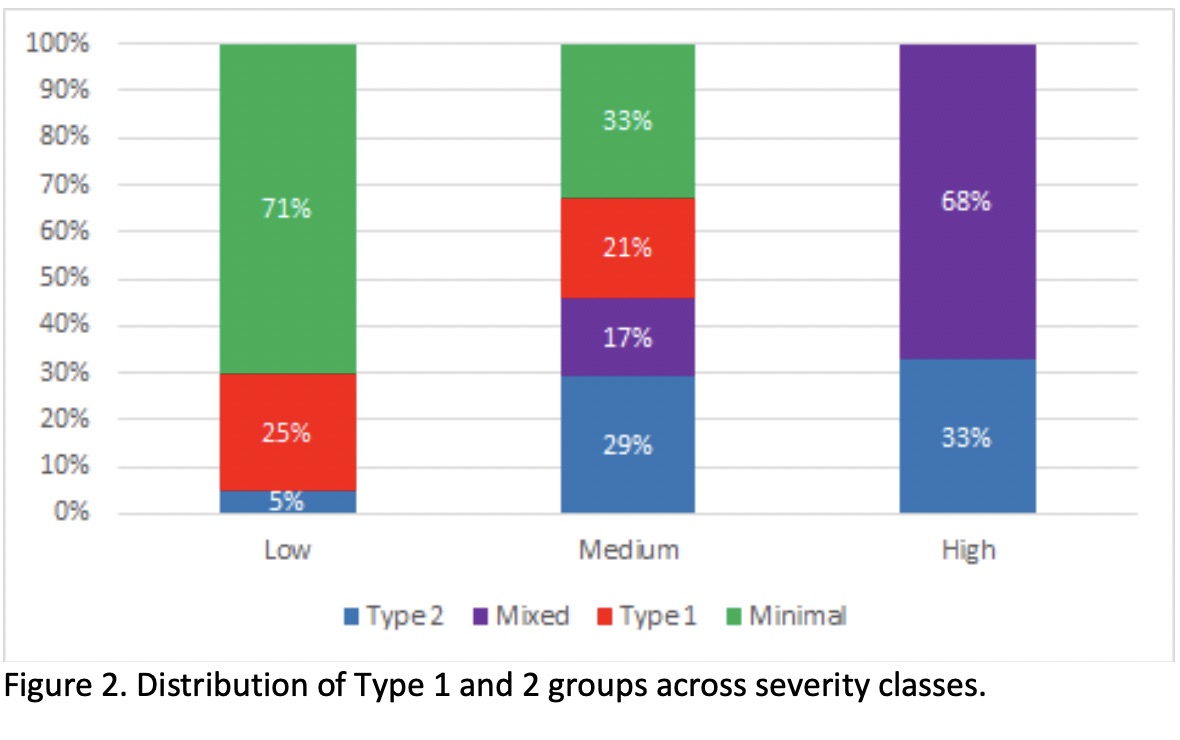 Figure 2. Distribution of Type 1 and 2 groups across severity classes.
Figure 2. Distribution of Type 1 and 2 groups across severity classes.
To cite this abstract in AMA style:
Eudy A, Reeve B, Coles T, Lin L, Rogers J, Criscione-Schreiber L, Doss J, Sun K, Sadun R, Katz P, Pisetsky D, Clowse M. Using Patient-Reported Outcomes Measures to Classify Patients with Systemic Lupus Erythematous [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/using-patient-reported-outcomes-measures-to-classify-patients-with-systemic-lupus-erythematous/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-patient-reported-outcomes-measures-to-classify-patients-with-systemic-lupus-erythematous/
