Session Information
Date: Monday, November 13, 2023
Title: (1200–1220) Patient Outcomes, Preferences, & Attitudes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease that has a large range of clinical manifestations, some of which can be severe. Reducing SLE flares leading to emergency room (ER) visits and hospitalizations is often difficult for clinicians given the heterogeneity of symptoms that can identify at-risk patients. The SLE Activity Questionnaire (SLAQ), a validated patient-reported instrument designed to screen disease activities in the clinical settings, may be a novel way to predict SLE-related healthcare utilization; but such association and application has not been studied and there have been few data to support its use in the clinical setting. The purpose of this analysis was to assess the patient-reported disease activity symptoms using SLAQ components in a population-based lupus cohort and develop a predictive model to identify patients at a higher risk for SLE-related hospitalization and ER visits.
Methods: This study used data from two surveys (2011-2013) of the Georgians Organized Against Lupus (GOAL) cohort, a Centers for Disease Control and Prevention supported population-based cohort of validated SLE patients in Atlanta who complete annual surveys, including sociodemographic and the SLAQ. This database was linked with the Georgia Hospital Discharge Database to obtain ER visits and hospitalizations within 6 months of each survey. An SLE-related hospitalization or ER visit is defined based on diagnosis of SLE-related condition in the primary position within 6 months of GOAL survey completion. The unadjusted association between SLAQ components and SLE-hospitalizations or ER visits was assessed using logistic regression to identify the strongest SLAQ predictors. A classification and regression tree (CART) model generated a decision tree for predicting SLE-hospitalization or ER risk based on the SLAQ components.
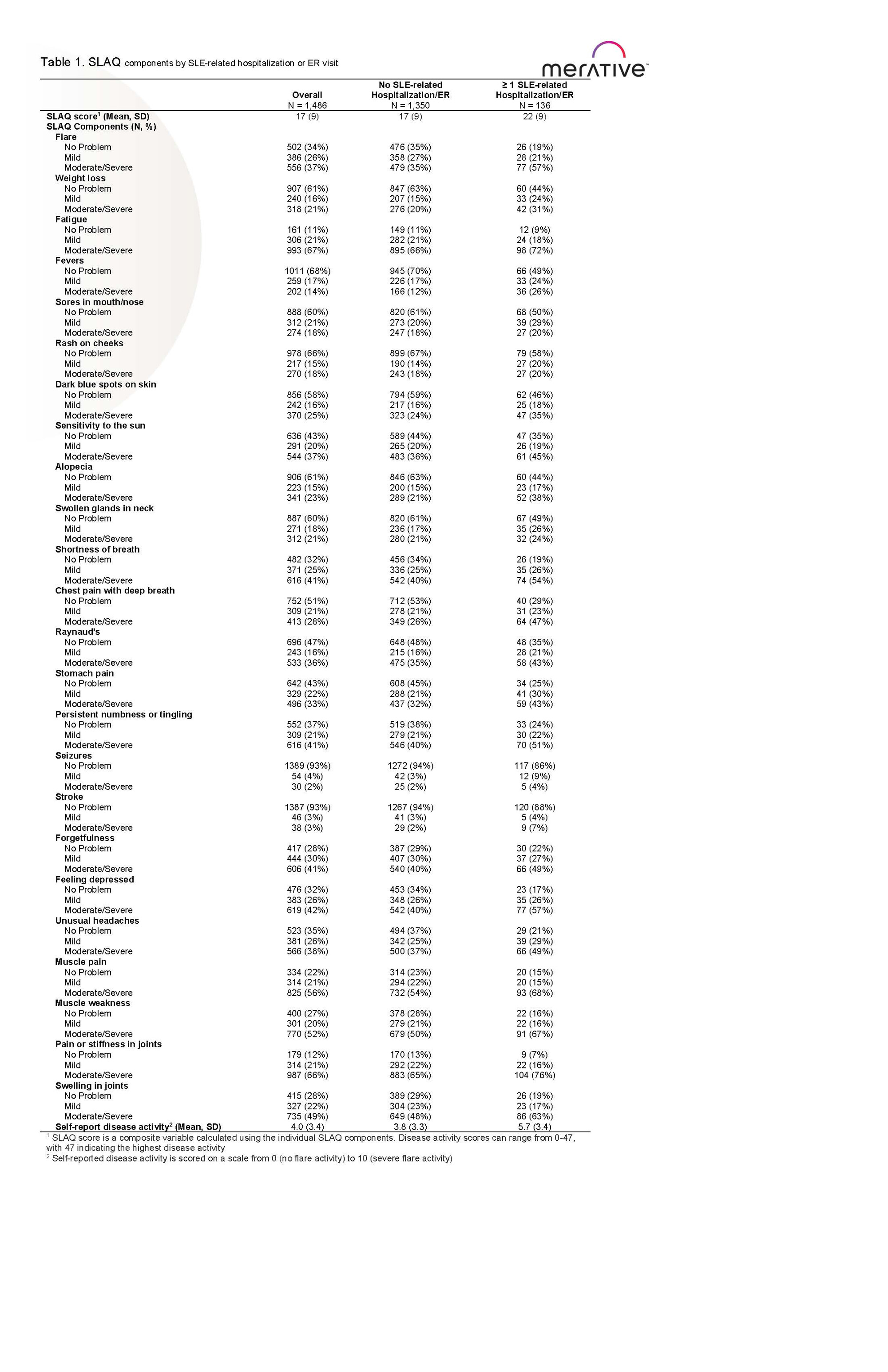
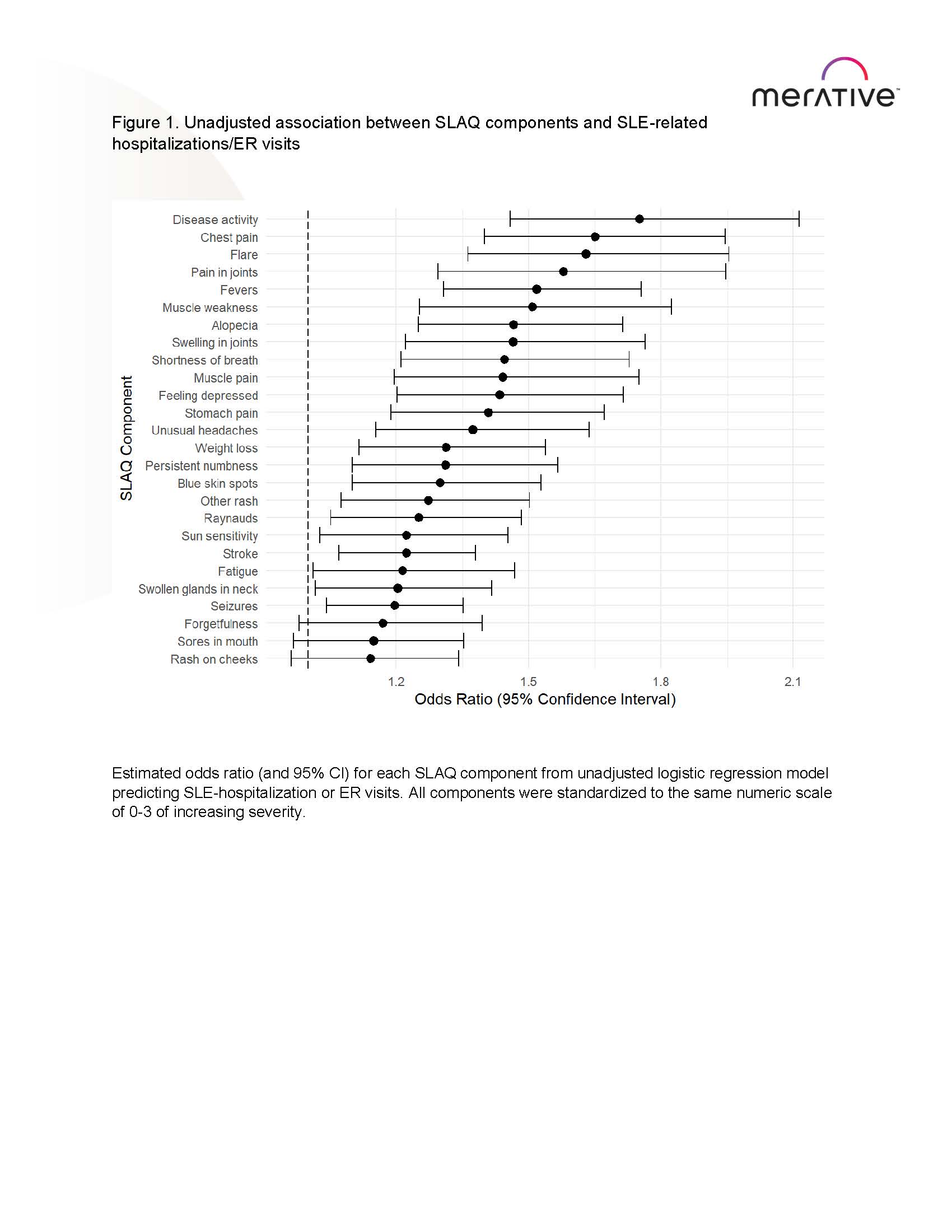
Results: Of the 1,486 GOAL participants, 136 (9.2%) had an SLE-related hospitalization or ER visit within 6-months of survey completion. The mean age at survey completion was 47 (SD: 13) years, 94% of patients were female, 78% of patients were Black, and had SLE for 14 (9) years. Patients with ≥1 SLE-related hospitalizations or ER visits had higher SLAQ scores than those without hospitalization (22 vs. 17; Table 1). The risk of SLE-related hospitalization or ER visit was higher among patients with higher disease activity scores, chest pain with deep breath, and those with more SLE flares (Figure 1). CART modeling suggests patients who had chest pain with deep breath and fevers as the high-risk group with 18.8% likelihood of an SLE-related hospitalization or ER visit in the next 6 months. The high-risk group have a 2-fold increased risk than the average patients (Pr=9.2%), and a 4-to-6-fold risk than those identified as low-risk (Pr=3.2-4.5%).
Conclusion: Patients who reported chest pain with deep breath and fevers were at the highest risk of having anSLE-related hospitalization or ER visit within 6 months. The inclusion of the SLAQ in routine care may provide physicians and patients with valuable information that could help mitigate healthcare utilization and improve outcomes.
To cite this abstract in AMA style:
Lim S, Wu S, Ross R, Bao G, Richards M, Palmer L, Bryant G. Using Patient-Reported Disease Activity in a Population-Based Cohort to Predict Systemic Lupus Erythematous Hospitalization and Emergency Room Visits [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/using-patient-reported-disease-activity-in-a-population-based-cohort-to-predict-systemic-lupus-erythematous-hospitalization-and-emergency-room-visits/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-patient-reported-disease-activity-in-a-population-based-cohort-to-predict-systemic-lupus-erythematous-hospitalization-and-emergency-room-visits/