Session Information
Date: Monday, November 18, 2024
Title: RA – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is among the most common extra-articular manifestations of RA, with symptomatic disease prevalent in approximately 10% of patients.1 Patients with symptomatic RA-ILD have an increased mortality rate, with a median survival of only 2.6 years from the time of ILD diagnosis1. While incidence of other extra-articular manifestations of RA has decreased over time with use of DMARDs,2 the incidence of RA-ILD has not. Studies have shown mixed associations ILD incidence and flares with use of the two most prescribed DMARDs, MTX and TNF-a inhibitors (TNFi)3-5. Furthermore, MTX has been associated with acute hypersensitivity pneumonitis (HP)6. Due to equivocal data, there is hesitancy among rheumatologists to prescribe MTX or TNFi in patients with pre-existing RA-ILD.
Methods: We conducted a nationwide survey among adult rheumatologists who were registered ACR members, examining practices surrounding MTX and TNFi use in RA-ILD. Of note, this survey was conducted prior to the publication of the 2023 ACR clinical practice guidelines for systemic autoimmune rheumatic disease (SARD)-associated ILD7.
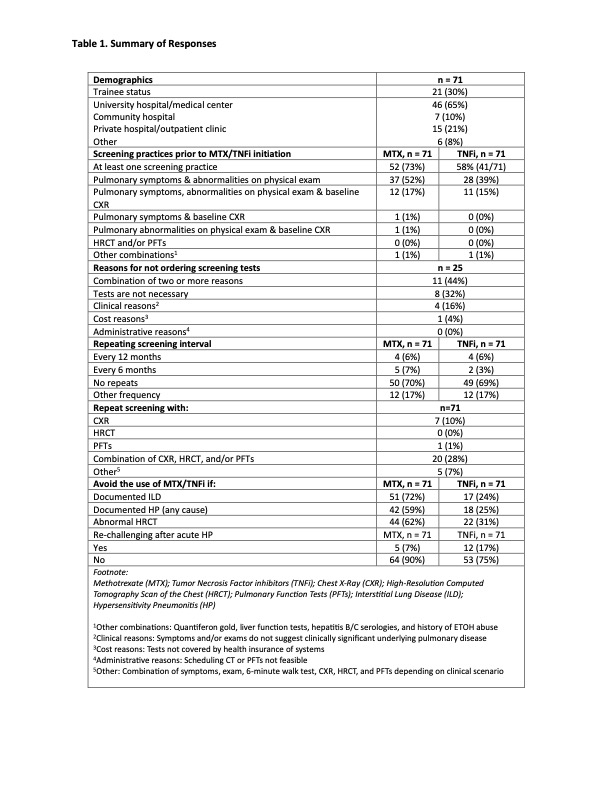
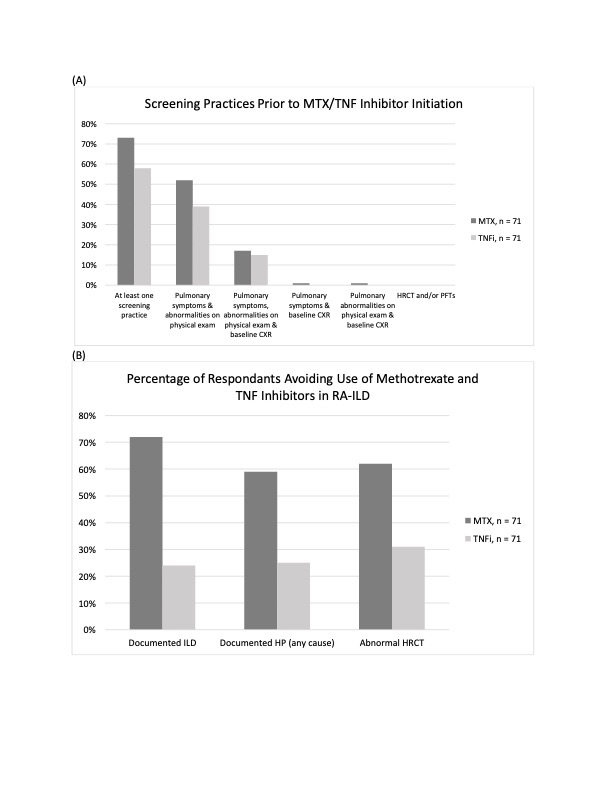
Results: The results of the survey are summarized in Table 1. The survey included multiple choice and free text questions. A total of 71 rheumatologists (out of 1,227 surveyed; 5.8% response rate) responded to the survey. Approximately half of the respondents stated they would screen with pulmonary symptoms and physical examination abnormalities prior to MTX and slightly fewer prior to TNFi initiation (Figure 1A). None stated they would screen with high-resolution computed tomography scan of the chest (HRCT) or pulmonary functions tests (PFTs). Approximately one-third stated they would not perform any screening measures as they did not believe the tests were necessary or due to clinical or cost reasons enumerated in Table 1. Most respondents stated they would avoid MTX in patients with documented ILD (72%), HP (59%), or abnormal HRCT (62%), while approximately one-quarter of respondents would avoid TNFi in such cases (24% for documented ILD, 25% for HP, 31% for abnormal HRCT) (Figure 1B). Those who would not avoid MTX/TNFi in ILD cited not having any robust data to suggest an association between MTX/TNFi and ILD. Most would not attempt to re-challenge with MTX or TNFi after an episode of HP because many other DMARDs are available. Some responded that they would re-challenge with a different TNFi.
Conclusion: In summary, we found that many respondents would perform a combination of pulmonary screening prior to initiation of MTX/TNFi, though most would not repeat screening, and that the majority would avoid MTX in patients with a documented history of ILD or HP. There are some notable differences between the ACR SARD-ILD guidelines and the survey data, such as respondents still favoring the use of CXR over HRCT as a screening tool. Furthermore, a lower-than-expected proportion stated they would screen with pulmonary symptoms/exam abnormalities, both low-cost options and standard care, prior to initiation of DMARDs. Therefore, it may be worth revisiting these practice trends after publication of the ACR SARD-ILD guidelines to evaluate practice changes.
A, Screening practices for RA-ILD prior to methotrexate or TNF inhibitor initiation among responding rheumatologists
B, Percent of responding rheumatologists who avoid methotrexate and TNF inhibitors in patients with RA-ILD
CXR = chest X-ray; HP = hypersensitivity pneumonitis; HRCT = high-resolution computed tomography scan of the chest; ILD = interstitial lung disease; MTX = methotrexate; RA-ILD = rheumatoid arthritis-associated interstitial lung disease; TNF = tumor necrosis factor; TNFi = tumor necrosis factor inhibitor
To cite this abstract in AMA style:
Park E, Iqbal R, Bernstein E, Giles J. Use of Methotrexate and TNF-α Inhibitors in Patients with Rheumatoid Arthritis-associated Interstitial Lung Disease: A Survey of Rheumatologists [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/use-of-methotrexate-and-tnf-%ce%b1-inhibitors-in-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease-a-survey-of-rheumatologists/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-methotrexate-and-tnf-%ce%b1-inhibitors-in-patients-with-rheumatoid-arthritis-associated-interstitial-lung-disease-a-survey-of-rheumatologists/