Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Infrared thermography (IRT) can detect joint inflammation in people with suspected inflammatory joint symptoms. Thus, IRT could be a helpful tool to assess joint pain in different clinical settings including primary care. We conducted a feasibility study to assess the use of IRT in the primary care clinic setting as a triage tool for the assessment of inflammatory arthritis in patients presenting with joint pain for the purpose of expediting rheumatology referral.
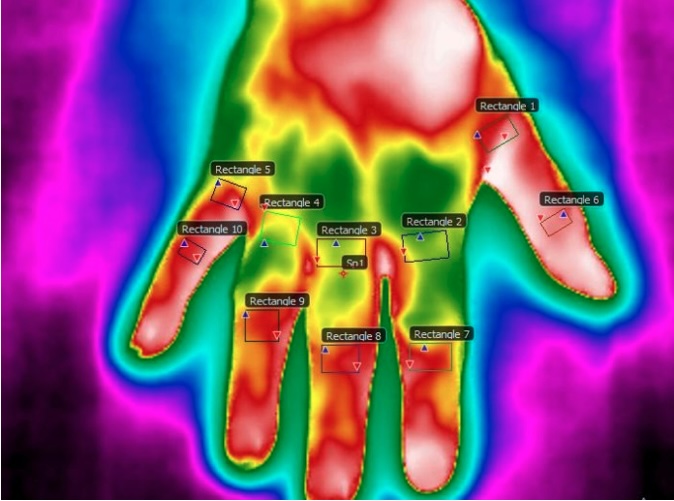
Methods: Eligible patients in this study were age >18 years, had prior/current wrist/hand/feet pain within the last 6 months (documented by PCP); patients previously seen by a rheumatologist were excluded. Using a previously established approach, IRT images from wrists/MCPs were obtained using a FLIR E75 3400 camera . A manual segmentation approach was employed on the images analyzed. (Figure 1) FLIR software was used to determine IRT temperature (°C) parameters including ROI maximum (max), minimum (min), mean (mean), center (center) and within-joint variability (STD). We previously established cut-off points for T mean and T center measurements based on ROC-AUC values using a logistic regression model to discriminate inflamed joints (power Doppler >1 on musculoskeletal ultrasound). Patients with temperatures above the cut off values (T center) for wrist and MCPs were referred. Electronic medical records reviewed following rheumatology visit on all recruited participants and information on rheumatology diagnosis as well as inflammatory and autoimmunity markers (e.g. CRP, ANA, RF, anti-CCP) were extracted. Descriptive statistics were used.
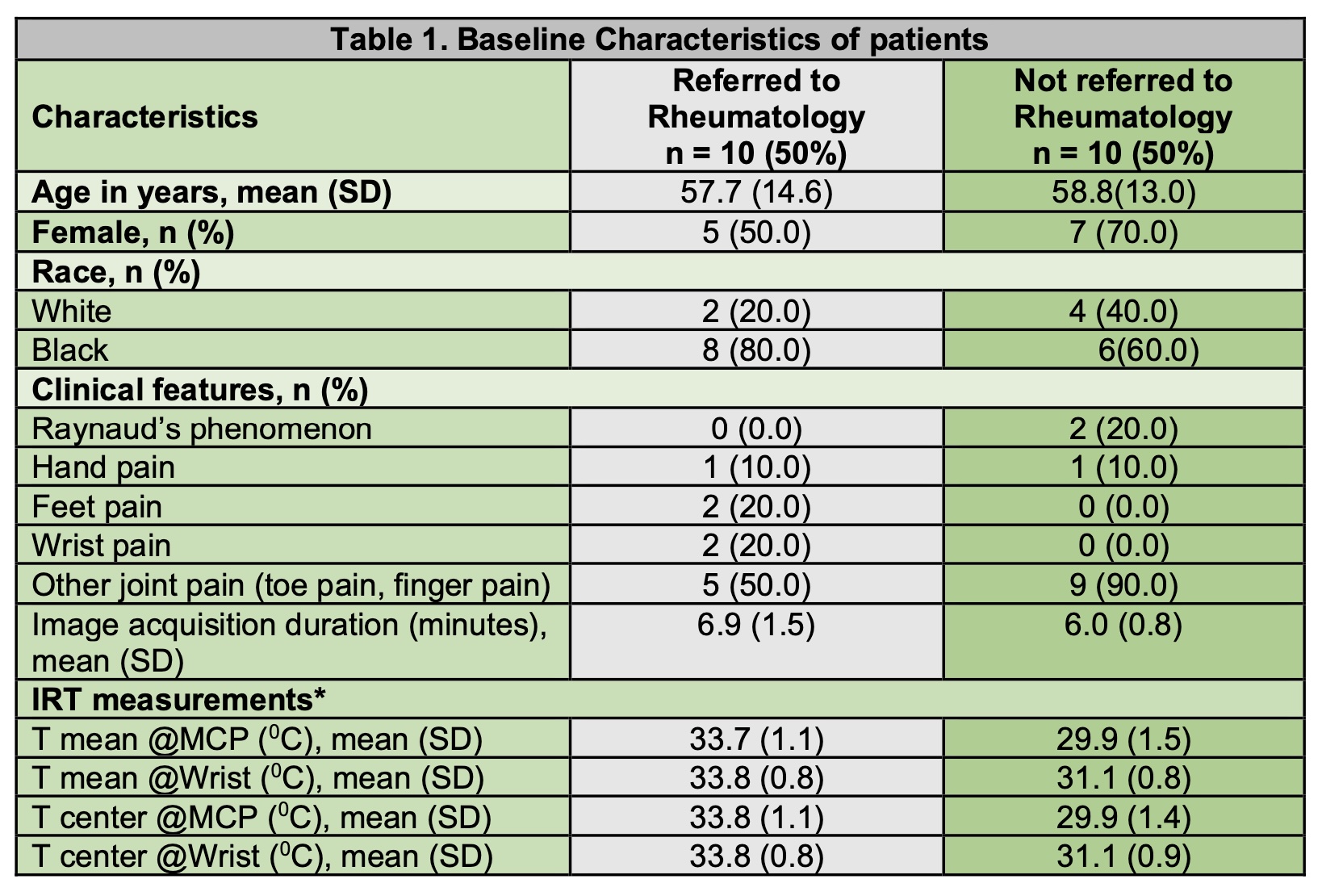
Results: A total of 20 patients were approached at their primary care visits between July 2023 and April 2024 with joint pain. Mean(SD) time required to obtain IRT images in the primary care visit was 6.9(1.5) minutes. Out of these, 10 patients met criteria based on T center values for MCPs and wrist (MCP: T center >32.93°C; wrist: T center >33.73°C) for rheumatology referral and were scheduled in the rheumatology clinic. Baseline characteristics of these patients that were referred to rheumatology vs not referred were: mean age (SD) 57.7(14.6) vs 58.8(13) years, female sex (%) 50 vs 70. (Table 1) Temperatures (SD) in both groups (referred vs not referred): T center MCP 33.8°C(1.1) vs 29.9°C(1.4) and T center wrist 33.8°C(0.8) vs 31.1°C(0.9). Eight out of ten referred were able to see a rheumatologist within 4 weeks after their PCP visit. Inflammatory markers in both groups were similar (referred vs not referred): ESR (17 vs 31.4 [normal 0-20 mm/hr]), CRP (13.5 vs 12.5 [normal 0-10.9 mg/L]). Only one patient had a positive RF (18) but no definite rheumatoid arthritis diagnosis. After rheumatology evaluation, 6 patients were diagnosed with osteoarthritis, 1 patient diagnosed with gout and 1 patient diagnosed with CPPD.
Conclusion: Thermography can be efficiently implemented during a primary care visit and could serve as an additional tool to improve clinicians’ confidence in the appropriateness of rheumatology referral. However, additional studies with larger sample sizes need to be conducted to optimize IRT utilization and thresholds to trigger referral and triage its appropriate timing.
To cite this abstract in AMA style:
Rosas chavez G, Aaron K, Curtis J, Begum R, Hughes L, Holder B, Danila M. Use of Infrared Thermography for Expedited Rheumatology Referral in a Primary Care Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/use-of-infrared-thermography-for-expedited-rheumatology-referral-in-a-primary-care-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-infrared-thermography-for-expedited-rheumatology-referral-in-a-primary-care-center/