Session Information
Session Type: Abstract Session
Session Time: 4:00PM-4:50PM
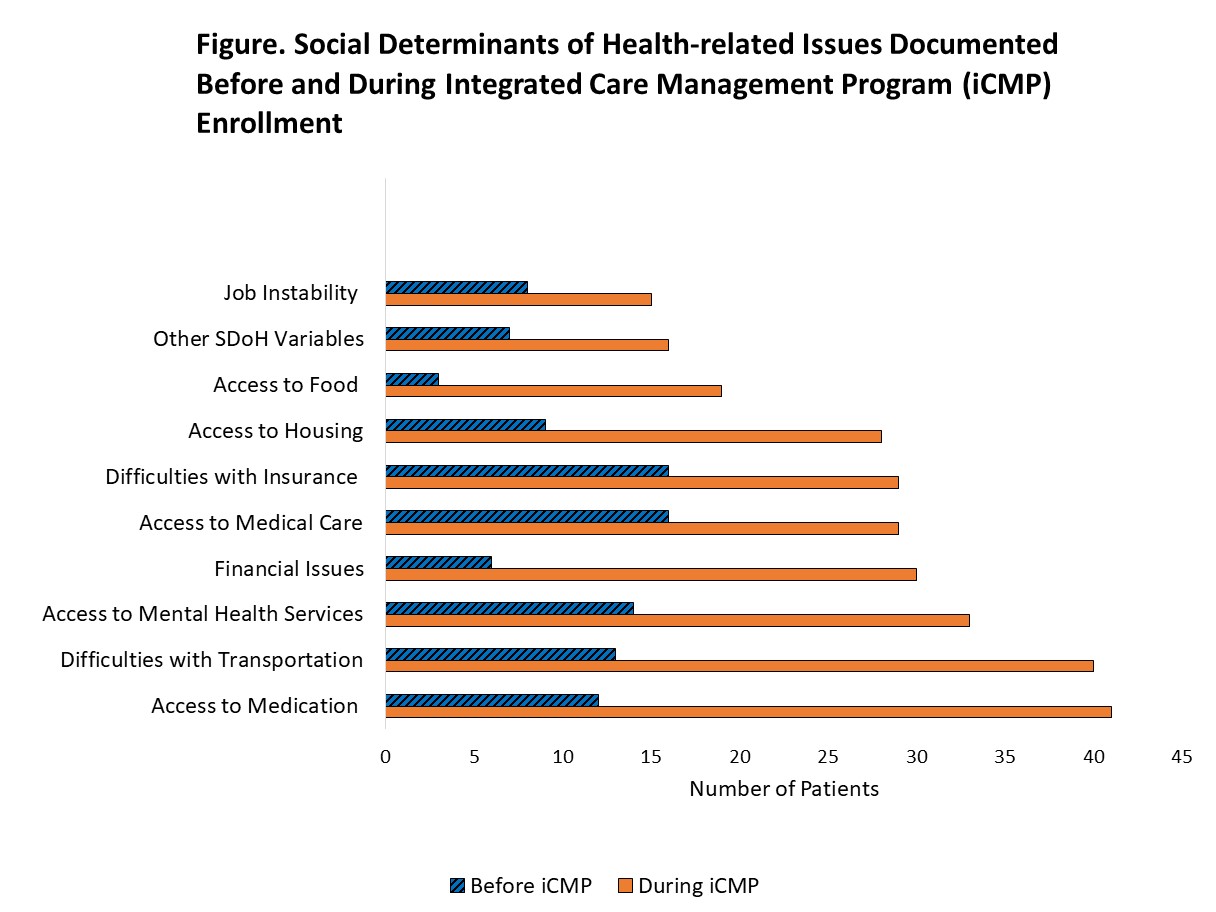
Background/Purpose: The burden of systemic lupus erythematosus (SLE) falls disproportionately on racial/ethnic minorities and individuals of lower socioeconomic status who often receive fragmented, inconsistent care. The Integrated Care Management Program (iCMP) enrolls patients at high risk for acute care use and adverse outcomes and connects them with a nurse and care team who help coordinate their medical care. We studied SLE patients enrolled in iCMP to understand whether social determinants of health (SDoH) needs such as food insecurity, housing instability, and financial constraints were prevalent in this population. We hypothesized iCMP teams would uncover and address SDoH issues that while likely present, would not have been documented before enrollment.
Methods: The iCMP enrolls the top 2% of medically and psychosocially complex patients within our multihospital primary care practices. Patients are identified by a system that incorporates clinical complexity, healthcare utilization indicators, and consultation with primary care providers, but does not explicitly factor in SDoH. Individuals with SLE enrolled in iCMP were identified with a validated machine learning algorithm (PPV=90%) and verified by chart review. We reviewed patients’ electronic health record encounters to identify SDoH needs prior to iCMP enrollment primarily using notes from physicians and social workers, and throughout enrollment using notes from iCMP nurses and team members.
Results: There were 69 patients with SLE enrolled in iCMP. Of these, 93% were female, 55% were white, 25% black, 3% Asian/Pacific Islander, 16% other/unknown race, and 21% were Hispanic. The mean duration of iCMP enrollment was 3.8 (SD 2.4) years. Prior to iCMP enrollment, 57% of the patients had documentation of ≥1 SDoH factor, compared to 94% during enrollment (Figure). The iCMP nurses addressed ≥1 SDoH factor for 81% of the SLE patients and completed high risks assessments for each patient. For these patients, iCMP nurses discussed and addressed multiple SDoH issues including medication access (66%), transportation (61%), insurance (50%), financial issues (48%), housing concerns (46%) and food insecurity (32%) (Table). The iCMP nurses connected 75% of these patients with additional resources, including social workers/mental health resources (58%), home health (43%) and elder care (14%) services, pharmacists (14%) and substance abuse programs (6%).
Conclusion: While SDoH-related issues were not used to identify patients for iCMP, the majority of enrolled high-risk, medically complex SLE patients had these needs. The iCMP nurses and care team members uncovered and addressed numerous SDoH-related concerns that while likely present, had not been documented prior to iCMP participation. As SDoH directly impact the care that patients access and the disproportionate burden of adverse outcomes among vulnerable populations, the healthcare system must develop and expand sustainable strategies like this integrated care management program to identify, document, and address these issues.
To cite this abstract in AMA style:
Taber K, Williams J, Huang W, McLaughlin K, Vogeli C, Cunningham R, Wichmann L, Feldman C. Use of an Integrated Care Management Program to Uncover and Address Social Determinants of Health for Individuals with Lupus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/use-of-an-integrated-care-management-program-to-uncover-and-address-social-determinants-of-health-for-individuals-with-lupus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-an-integrated-care-management-program-to-uncover-and-address-social-determinants-of-health-for-individuals-with-lupus/