Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: To inform guidance for cancer surveillance in patients with idiopathic inflammatory myositis (IIM), we conducted a retrospective cohort study in a single tertiary referral center to evaluate the use and yield of computed tomography (CT) for cancer surveillance within distinct myositis-specific autoantibody strata from 2007 through 2020.
Methods: In 2020, we reviewed the electronic medical records of all patients who previously enrolled in our Myositis Research Registry to identify those who met the following criteria: (i) Probable or definite DM/PM by Peter and Bohan, (ii) IMNM by the 2003 ENMC Criteria, (iii) Classic DM rash (Gottron’s/heliotrope) and consistent histopathology on skin biopsy. Myositis specific and associated autoantibodies were assayed using Euroimmun line blot (16 Ag IgG), ELISA (anti-Mi2 and anti-TIF1ƴ [MBL], anti-HMGCR [INOVA Diagnostics]), and in-house immunoprecipitation (anti-NXP2). We also reviewed their charts and outside medical records for any CT chest and abdomen/pelvis studies ordered for cancer surveillance/screening purposes. Our myositis center’s strategy for malignancy screening/surveillance includes at least one CT chest, abdomen, and pelvis upon IIM diagnosis. Data on CT imaging was collected with researchers blinded to both myositis-specific autoantibody and cancer status. Two time periods were analyzed: Cancer screening tests performed (i) after cohort enrollment, and (ii) after IIM-symptom onset, both through 12/31/2020.
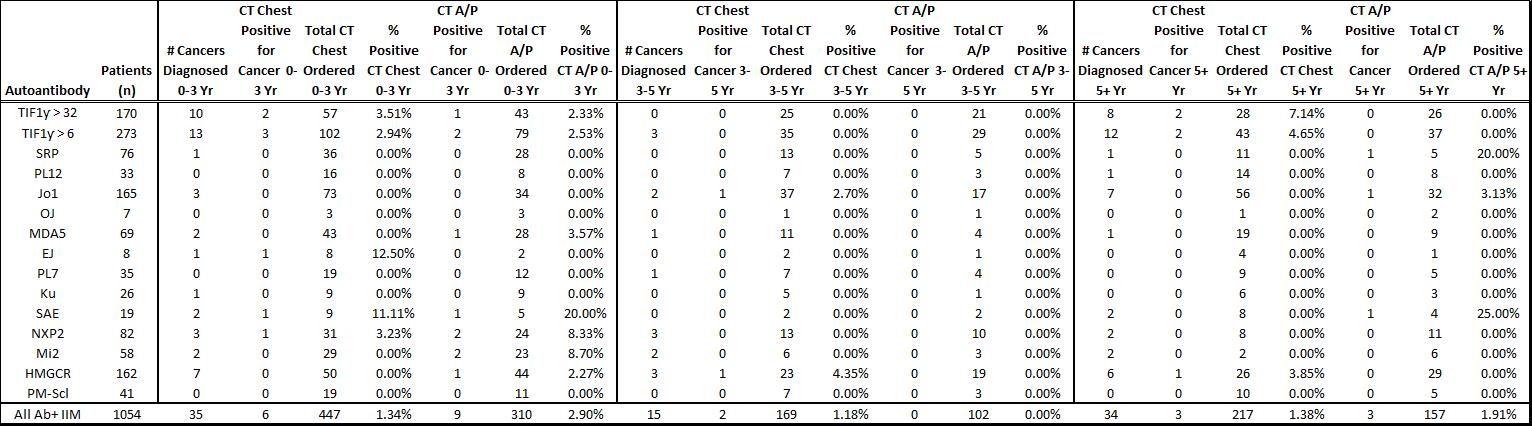
Results: Among 1174 patients, 1054 patients had at least one myositis specific or associated autoantibody. From cohort enrollment onwards, the number of cancers that occurred within 0-3 yrs, 3-5 yrs, and >5 yrs after IIM symptom onset was 35, 15, and 34, respectively. The number/% of CT chest scans that were positive for cancer were 6/1.34% (0-3 yrs), 2/1.18% (3-5 yrs), and 3/1.38% ( >5 yrs). The number/% of CT a/p positive for cancer was 9/2.90% (0-3 yrs), 0/0% (3-5 yrs), and 3/1.91% ( >5 yrs). Of the 35 cancers diagnosed within 0-3 yrs from IIM symptom onset, more than half were diagnosed by methods other than CT chest, abdomen and pelvis imaging. Amongst 273 anti-TIF1g-positive patients, 181 CT chest or a/p scans were performed, 5 (2.7%) of which were positive within 0-3 yrs. In contrast, amongst 248 patients with Jo1, PL12, PL7, OJ, or EJ autoantibodies, 178 CT chest or a/p scans were performed, 1 (< 1%) of which was positive.
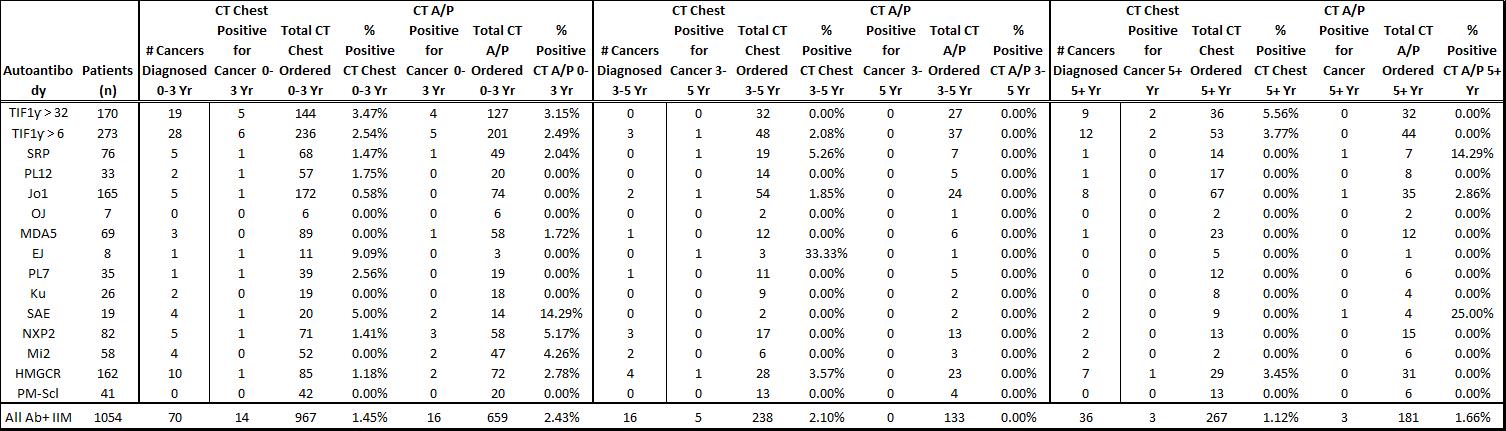
From IIM symptom onset onwards, the number of IIM patients diagnosed with cancer that occurred within 0-3 yrs, 3-5 yrs, and >5 yrs after IIM symptom onset was 70, 16, and 36. The percent of screening/surveillance CT chest and CT a/p scans that were positive for cancer was comparable to the time window from cohort enrollment onwards (Table 2).
Conclusion: In a tertiary referral center population, the number of patients needed to be screened by CT imaging to detect one cancer within the first 3 yrs of IIM was approximately 70 for CT chest and 40 for CT a/p. CT imaging is of higher yield in patients with anti-TIF1ƴ antibodies compared to patients with antisynthetase autoantibodies. Whether CT imaging leads to improvement in cancer or IIM outcomes remains to be determined. Funded in part by NIAMS K23AR075898.
To cite this abstract in AMA style:
Mecoli C, Chee B, Wang X, Chen M, Kelly W, Platz E, Casciola-Rosen L, Christopher-Stine L, Shah A. Use and Yield of Computed Tomography as a Cancer Surveillance Method in Idiopathic Inflammatory Myositis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/use-and-yield-of-computed-tomography-as-a-cancer-surveillance-method-in-idiopathic-inflammatory-myositis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-and-yield-of-computed-tomography-as-a-cancer-surveillance-method-in-idiopathic-inflammatory-myositis/