Background/Purpose: Glomerulonephritis is common in ANCA-associated vasculitis (AAV), but non-invasive tools for early detection of renal involvement suffer from low sensitivity (red blood cell casts) or low specificity (hematuria). We investigated four urinary proteins as potential markers of active renal AAV: alpha-1 acid glycoprotein (AGP), kidney injury molecule-1 (KIM-1), monocyte chemoattractant protein-1 (MCP-1), and neutrophil gelatinase-associated lipocalin (NGAL).
Methods: Patients with active renal AAV (n=20), active non-renal AAV (n=16), and AAV in long-term remission (n=14) were identified within a longitudinal cohort, in which detailed clinical assessment and urinalysis results had been recorded at every visit. Biomarker concentrations were measured by ELISA and normalized for urine creatinine. Marker levels during active AAV were compared to baseline remission levels determined from 1-4 remission visits for each patient. Areas under receiver-operating characteristic curves (AUC), sensitivities, specificities, and likelihood ratios (LR) comparing disease states were calculated. Generalized linear models were used to assess the effects of proteinuria, treatment, and other variables on marker levels.
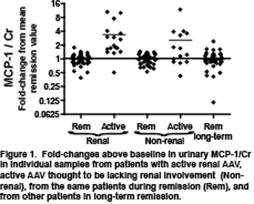
Results: Baseline biomarker levels varied among patients. All four markers increased during renal flares (P<0.05). MCP-1 discriminated best between active renal disease and remission: a 1.3-fold increase in MCP-1 per mg creatinine had 94% sensitivity and 89% specificity for active renal disease (AUC=0.93, positive LR 8.5, negative LR 0.07; see Figure 1). However, increased MCP-1 also characterized 50% of apparently non-renal flares. Changes in non-specific proteinuria did not account for the association of MCP-1 with active renal disease, nor did changes in treatment. Change in AGP, KIM-1, or NGAL showed more modest ability to distinguish active renal disease from remission (AUC 0.71-0.75). Hematuria was noted during 63% of active renal episodes, but also during 38% of non-renal flares and 25% of remission visits.
Conclusion: An increase in urinary MCP-1 may signal renal involvement in AAV. In contrast to a previous report, MCP-1 was imperfect in distinguishing active renal AAV from remission and was also elevated in cases in which renal involvement was thought to be absent. Either MCP-1 showed poor specificity for renal disease, or it improved sensitivity for detecting it, and urinalyses indicated that non-invasive assessment of active renal disease might be challenging in this cohort. AGP, KIM-1, and NGAL, despite being among the most promising markers in other kidney diseases, have lower prospects for clinical use in AAV.
Disclosure:
J. G. Lieberthal,
None;
D. Cuthbertson,
None;
S. Carette,
None;
G. S. Hoffman,
None;
N. A. Khalidi,
None;
C. L. Koening,
None;
C. A. Langford,
None;
K. Maksimowicz-McKinnon,
None;
P. Seo,
None;
U. Specks,
None;
S. R. Ytterberg,
None;
P. A. Merkel,
None;
P. A. Monach,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/urinary-biomarkers-in-vasculitis-associated-with-anti-neutrophil-cytoplasmic-antibodies/