Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Circulating monocytes are divided into three subsets: classical, intermediate, and non-classical monocytes. Monocytes egress from the bone marrow as classical monocytes and develop into intermediate and later non-classical monocytes. In patients with systemic lupus erythematosus (SLE), the proportion of non-classical monocytes is increased in the peripheral blood and kidneys in case of glomerulonephritis. However, the biology of non-classical monocytes in patients with SLE and their implications in the disease process are not fully characterized.
Methods: Peripheral blood mononuclear cells (PBMC) were isolated from patients with SLE (defined by the 2019 EULAR/ACR criteria; n=20), healthy controls (n=20), and patients with connective tissue diseases other than SLE (n=10). PBMC were stained for CD14, CD16, and CD115 and analyzed by flow cytometry. In additional experiments, mitochondrial membrane potential and mitochondrial reactive oxygen species were measured by flow cytometry, expression of miR146a was quantified by RT-qPCR. All patients and blood donors gave written informed consent and the study was approved by the ethical review board of the University of Freiburg.
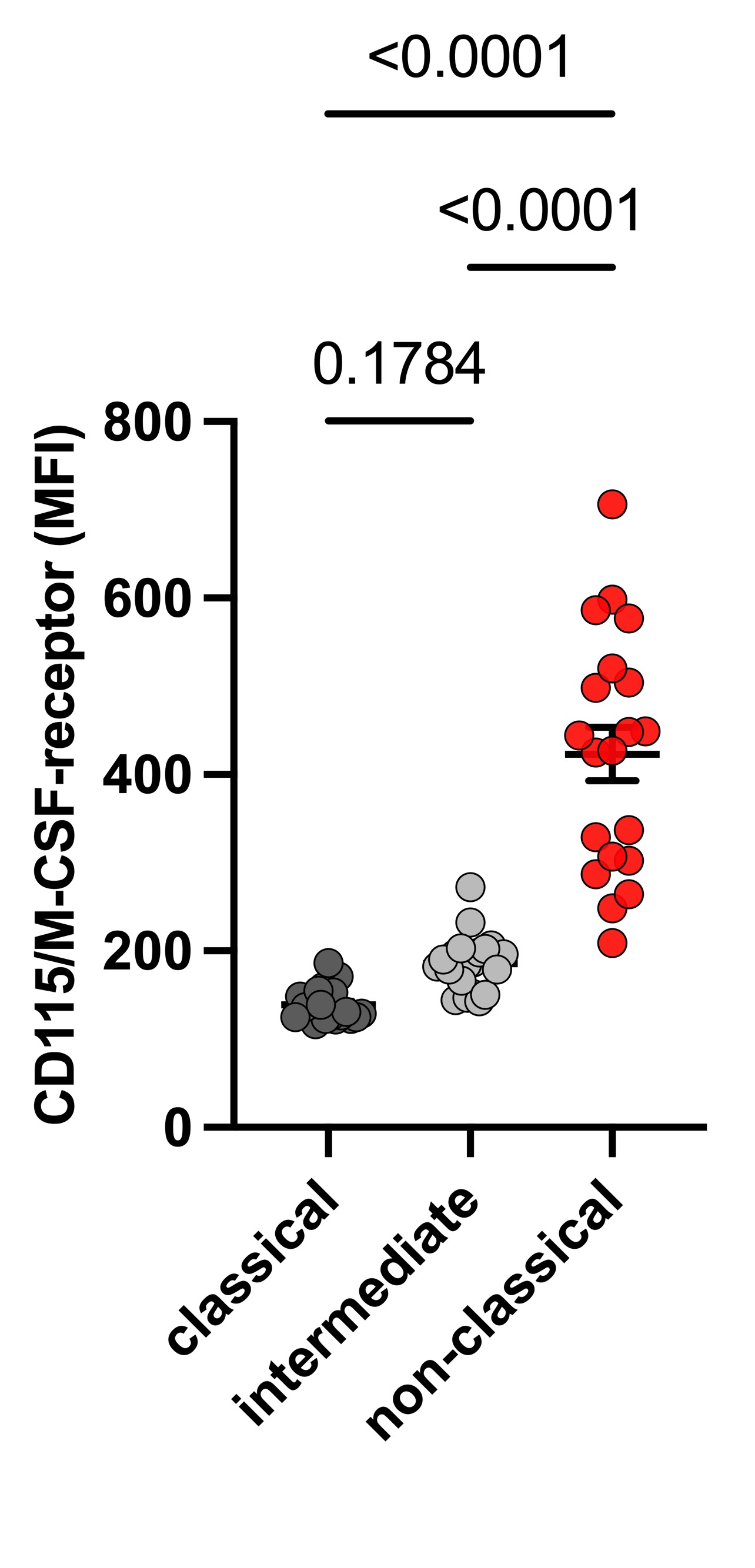
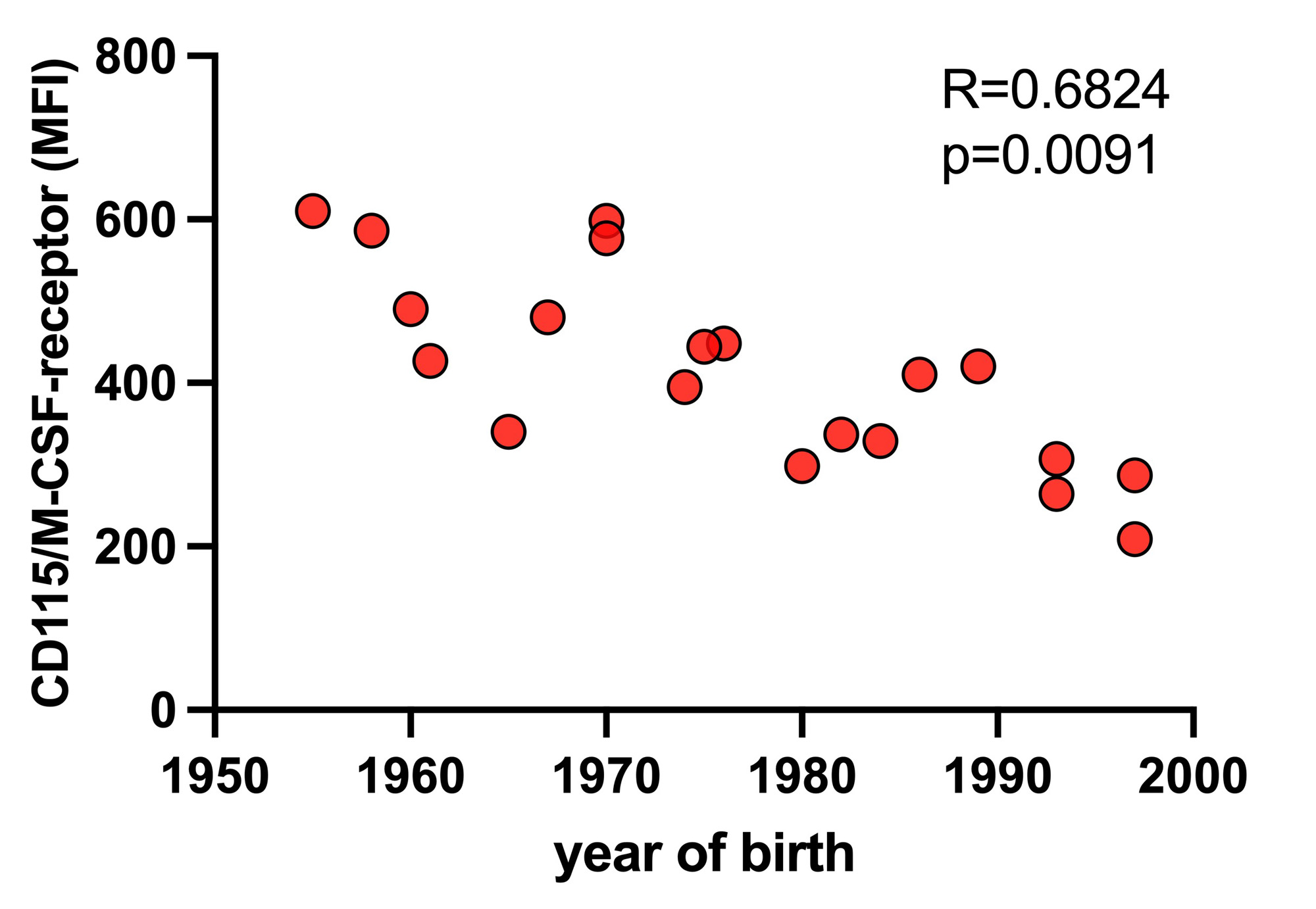
Results: Surface expression of CD115, the receptor for macrophage colony stimulating factor (M-CSF), a key survival factor for myeloid cells, is markedly upregulated on non-classical monocytes from patients with SLE. While CD115 is almost absent on the classical monocyte subset and intermediate monocytes show low levels of CD115, only non-classical monocytes exhibit a relevant surface expression of the M-CSF receptor (Figure 1). Non-classical monocytes from SLE patients increase their CD115 expression not only in comparison with healthy age-matched controls (p=0.004) but also compared to patients with connective tissue diseases other than SLE (p=0.009), identifying the upregulation of the M-CSF receptor as biological signature of non-classical monocytes in SLE. These CD115+ monocytes in SLE patients display a senescent cell phenotype with increased mitochondrial membrane potential (p=0.012), higher production of mitochondrial reactive oxygen species (p=0.021) and upregulation of the senescence marker miR146a (p=0.008). When investigating CD115 expression in different age groups in healthy individuals, CD115 receptor levels on non-classical monocytes were age-dependent with low levels on cells from young adults and significantly higher levels in individuals over 50 years of age (Figure 2). Thus, the upregulated CD115 expression of non-classical monocytes from young SLE patients was indicative for premature monocyte aging in line with the upregulation of senescence markers in those cells.
Conclusion: We identified the upregulation of the M-CSF receptor (CD115) as a biological signature of non-classical monocytes from SLE patients. CD115+ non-classical monocytes are increased only in the peripheral blood of patients with SLE and not in patients with other connective tissue diseases and display a senescent phenotype indicative of premature monocyte aging in SLE.
To cite this abstract in AMA style:
Zeisbrich M, Finzel S, Venhoff N, Voll R. Upregulation of the M-CSF Receptor on Non-Classical Monocytes from SLE Patients as an Indicator for Premature Monocyte Aging [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/upregulation-of-the-m-csf-receptor-on-non-classical-monocytes-from-sle-patients-as-an-indicator-for-premature-monocyte-aging/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/upregulation-of-the-m-csf-receptor-on-non-classical-monocytes-from-sle-patients-as-an-indicator-for-premature-monocyte-aging/