Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Sarcoidosis is a complex, multisystemic disorder predominantly affecting the pulmonary system but can also involve extra-pulmonary organs such as the heart. Mortality in sarcoidosis varies from < 1% to approximately 8% and depends largely on the organ affected, with cardiac sarcoidosis (CS) accounting for nearly two-thirds of deaths. The aim of this study was to assess the prevalence, in-hospital mortality, and readmission rates in patients admitted with cardiac sarcoidosis (CS) vs pulmonary sarcoidosis (PS).
Methods: The National Readmission Database, between years 2016-2020, was used to identify cardiac and pulmonary sarcoidosis admissions with the following ICD-10 codes D860, D862, and D8685. Patients under 18 years of age were excluded. All statistical analyses were performed using Stata 18.0 software.
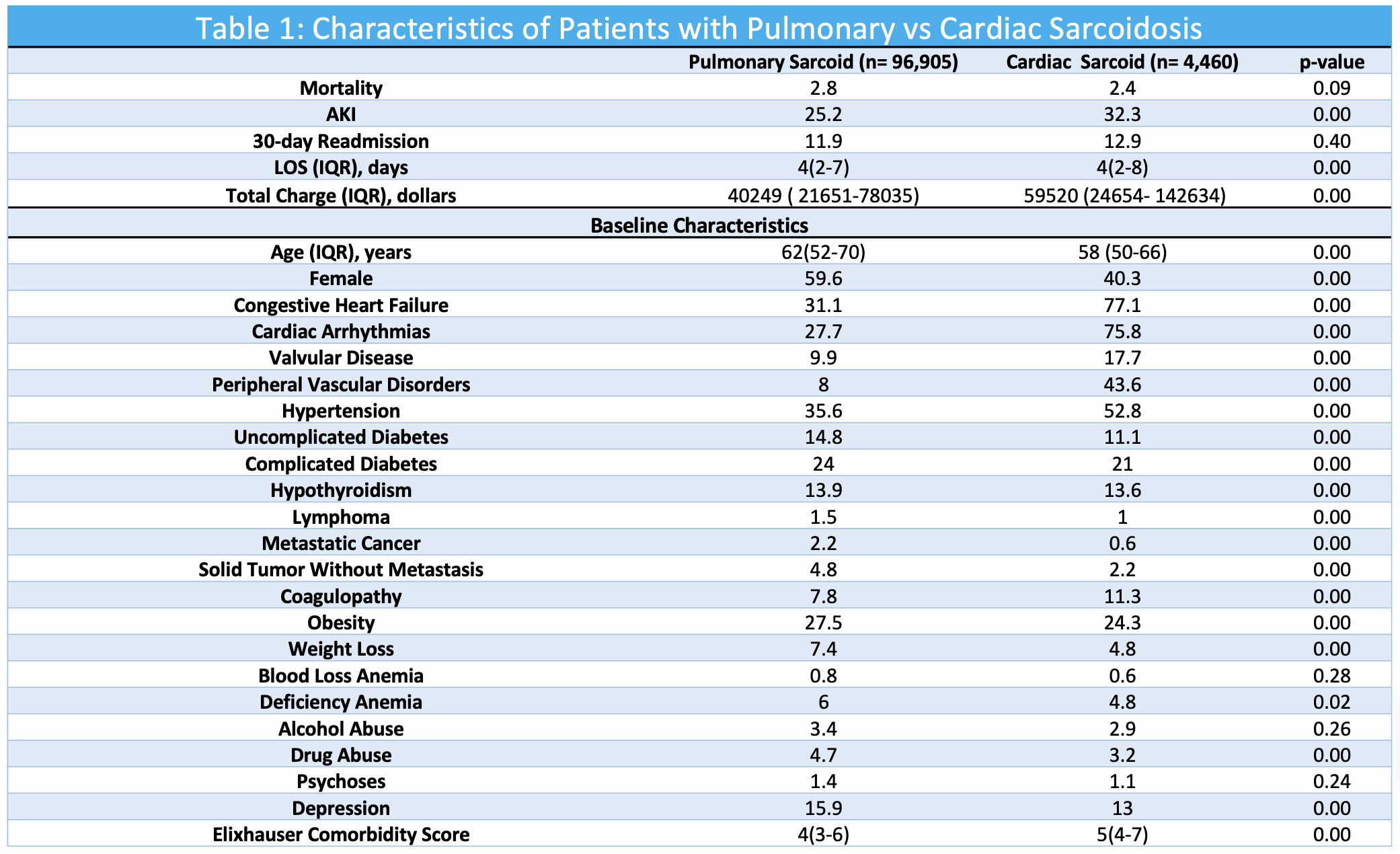
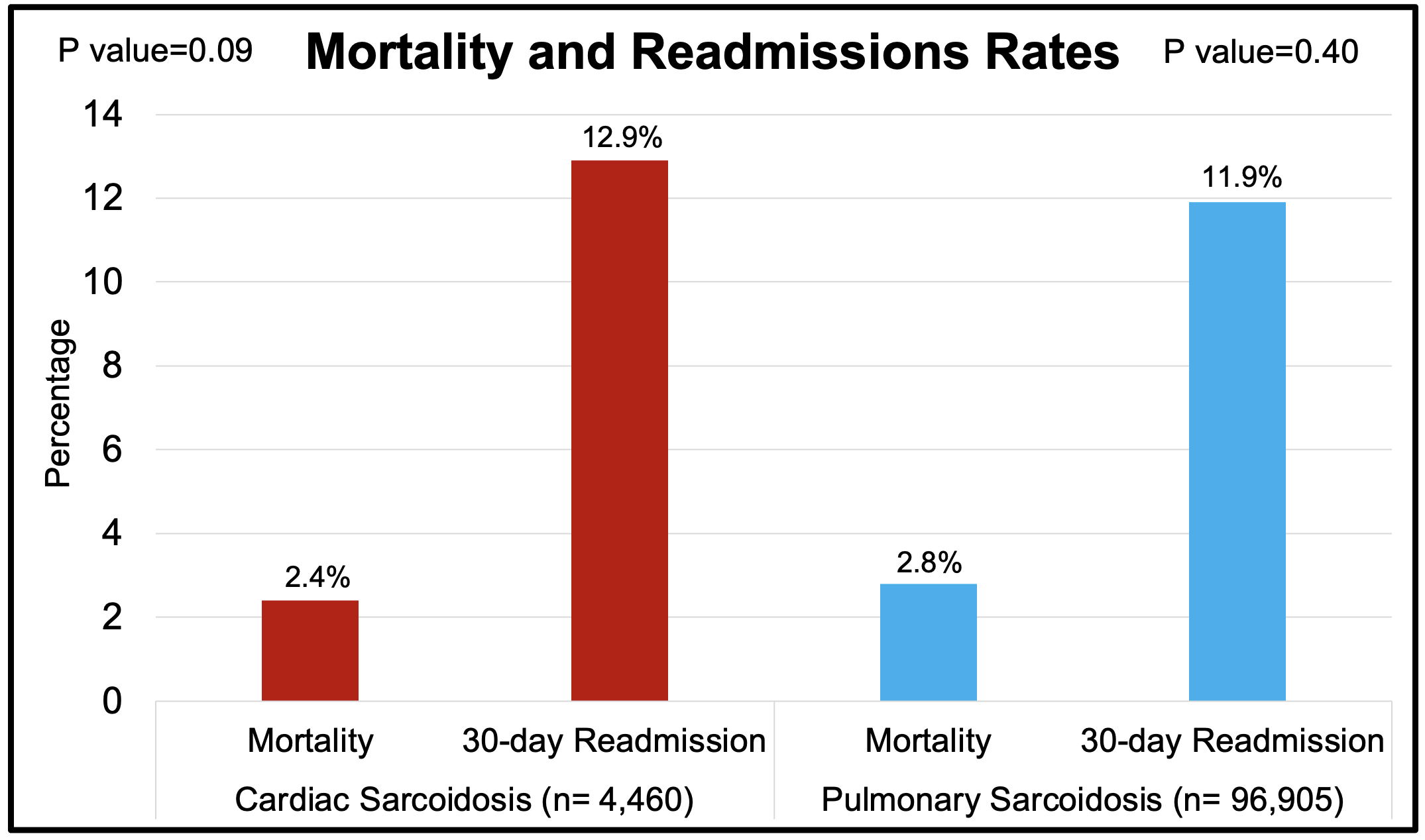
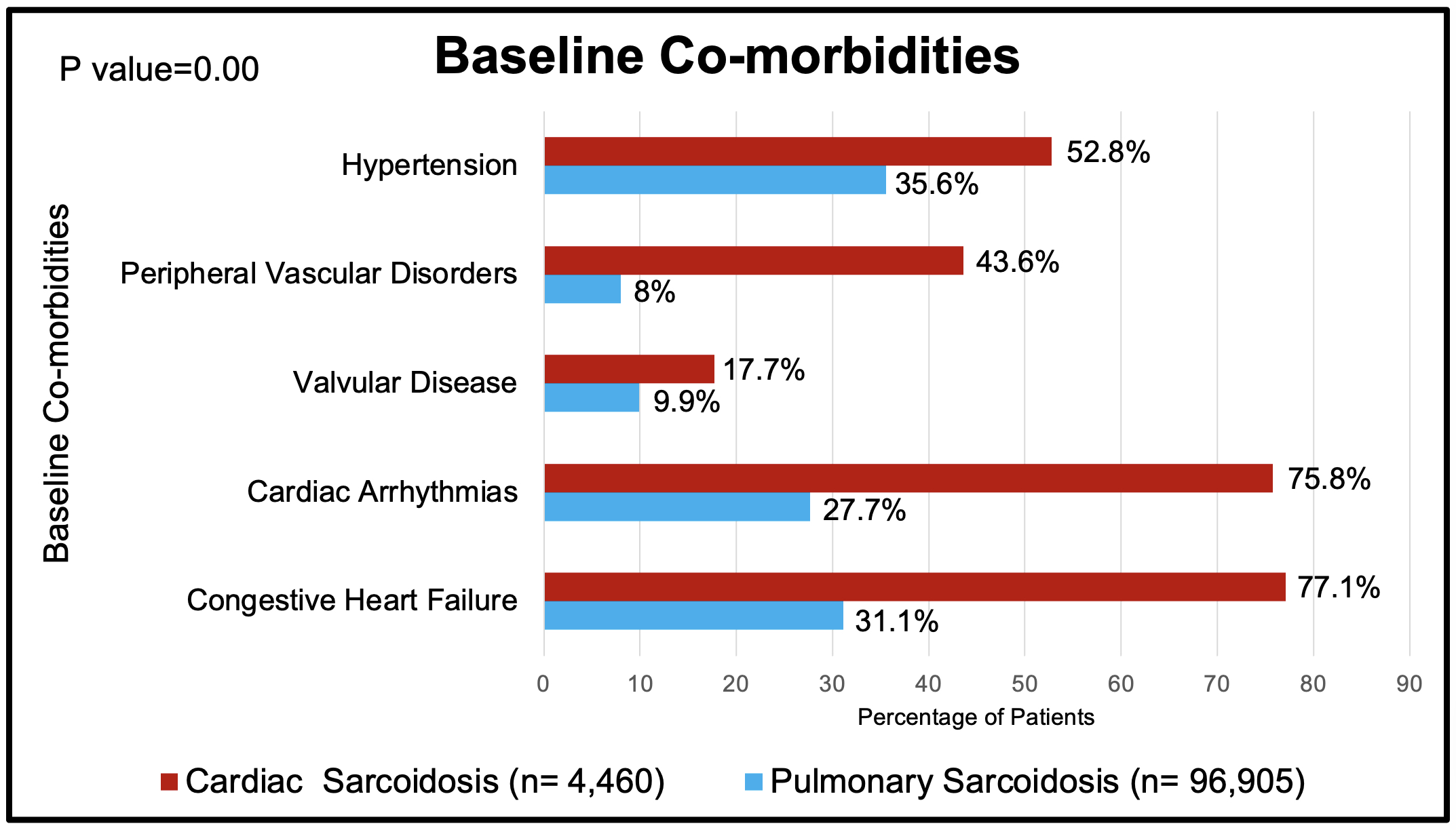
Results: From 2016 to 2020, 103,403 patients were identified; 6.3% had CS (n=6,498, mean age: 58 years, female=40.9%) while 93.7% had PS (n=96,905, mean age: 62 years, female=59.6%). At baseline, CS patients had significantly higher rates of co-morbidities including congestive heart failure (77.8% vs 31.1%, p< 0.001), cardiac arrhythmias (73.7% vs 27.7%, p< 0.001), valvular disease (17.9% vs 9.9%, p< 0.001), peripheral vascular disorders (42.6% vs 8.0%, p< 0.001), and complicated hypertension (52.2% vs 34.4%, p< 0.001). Despite a lower prevalence of patients with CS, we observed a similar in-hospital mortality rate between CS vs PS patients (2.4% vs 2.8%, p=0.219). Moreover, 30-day readmissions were comparable between the two groups (12.5% vs 11.9%, p=0.4). The most common causes of 30-day readmission in CS were heart failure exacerbation (55.62%), sepsis (11.99%), and cardiac implantable electronic device complications (2.74%). Amongst patients with PS, the most common causes of readmission were sepsis (15.46%), heart failure exacerbation (7.13%), and acute on chronic respiratory failure with hypoxia (5.44%). While length of stay was grossly comparable between the two groups, we observed that patients with CS had higher total charges as compared to their counterparts with PS ($59520 vs $40249, p< 0.001).
Conclusion: Despite a significantly lower prevalence of CS, these patients had a higher cardiovascular disease burden at baseline, with similar rates of in-hospital mortality and 30-day readmissions when compared to patients with PS. The results from this study shed light on the increased acuity, complexity, and higher health care costs in patients with CS when compared to PS despite its lower prevalence. Further studies are needed to better understand this disease process to improve outcomes.
To cite this abstract in AMA style:
Chaudhary S, Gokul K, Patel K, Bhimani S, Deshpande Y, Kilian A, Nayak R, Mikhalkova D, Rojulpote C. Understanding the Prevalence, In-Hospital Mortality and Readmission Rates Amongst Pulmonary vs Cardiac Sarcoidosis Patients: Insights from a Nationwide Registry [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/understanding-the-prevalence-in-hospital-mortality-and-readmission-rates-amongst-pulmonary-vs-cardiac-sarcoidosis-patients-insights-from-a-nationwide-registry/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/understanding-the-prevalence-in-hospital-mortality-and-readmission-rates-amongst-pulmonary-vs-cardiac-sarcoidosis-patients-insights-from-a-nationwide-registry/