Session Information
Date: Monday, November 14, 2022
Title: Abstracts: Vasculitis – Non-ANCA-Associated and Related Disorders II
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
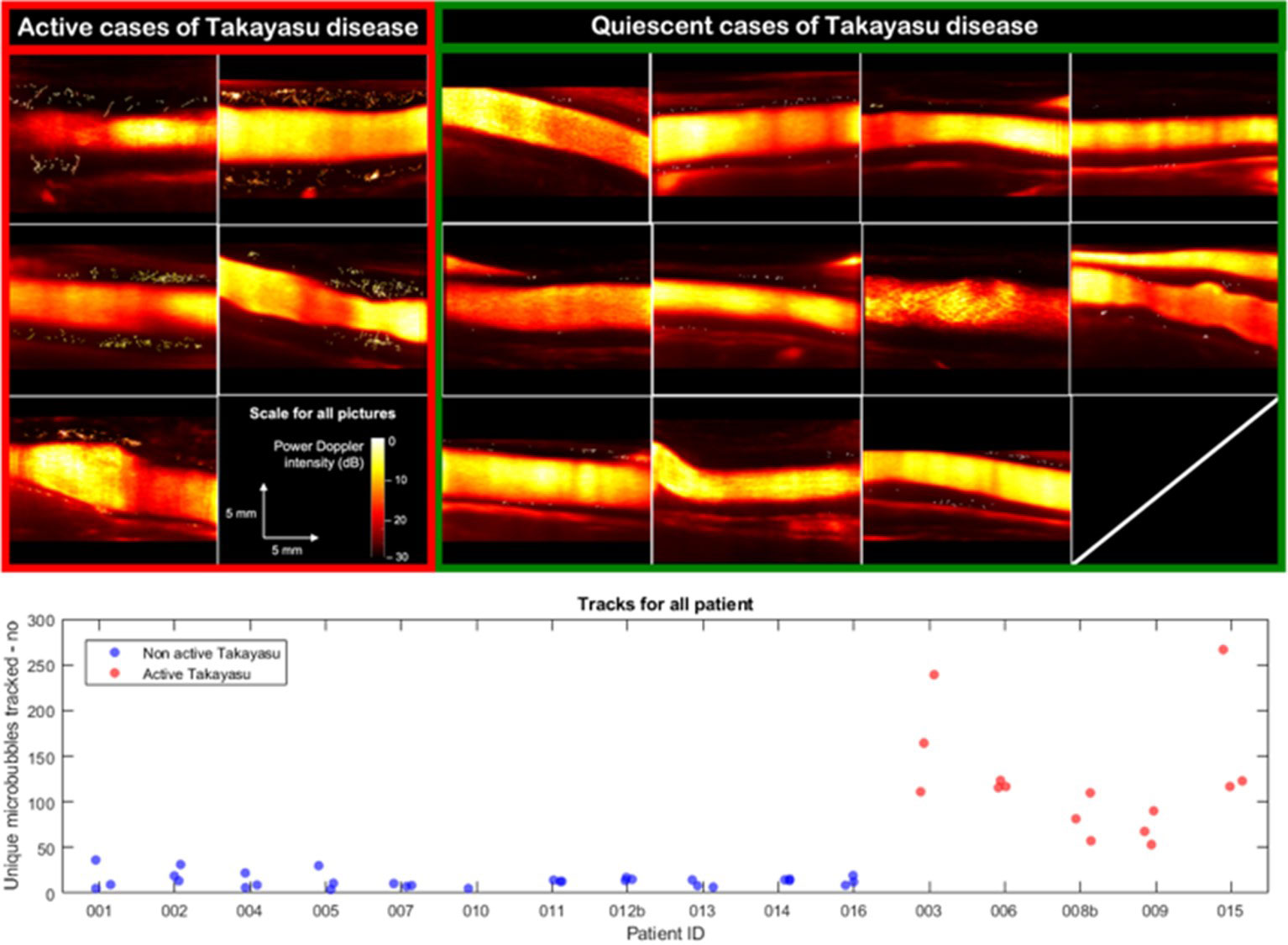
Background/Purpose: Use of sulphur hexafluoride microbubbles (MB) with ultrasound allow to assess arterial wall vascularization through signal enhancement. The use of ultrafast imaging with MB super-localization provides access to ultrasound localization microscopy (ULM) and thus to visualize carotid vasa vasorum in vivo. We aim to perform vasa vasorum imaging within the carotid wall in Takayasu’s arteritis and to provide a correlation with disease’s activity.
Methods: Patients with Takayasu’s arteritis were consecutively included in the French national referral centre for rare vascular diseases. Assessment of activity was performed using NIH activity index, with measurement of biological inflammation, morphological assessment by computed tomography (CT) angiography, and 18-fluorodeoxyglucose CT scan. Ultrafast ultrasound imaging was performed with a 7 MHz central frequency linear probe. A dedicated contrast imaging sequence (plane waves with 8 angles, frame rate 500 Hz, voltage 8 V, duration of 8 s), coupled with the intravenous injection of sulphur hexafluoride MB allow us to store the raw radio frequency data of the MB passage. After a pre-processing step to accumulate frames properly including a frames selection and a movement correction, the MB were localized then tracked, allowing reconstruction of the vasa vasorum. The inflammation was quantified through MB tracked and normalized for inter acquisition comparison.
Results: Sixteen patients have been included, among whom 5 patients (median age 35.8 [24.5–46.0] years, 3 women) had active disease and 11 patients (37.2 [31.7–47.3] years, 9 women) had quiescent disease. The passage of MB allowed to see microvessels within the carotid arterial wall for active cases. The number of MB detected per second in the wall was 118 [80–169] for active cases versus 13 [10–15] for quiescent cases (p=0.0005). The sum of the length of the tracks, i.e. the MB path per second of acquisition, was computed with a significant difference between the two groups with 43.0 mm [32.9–65.5] in active cases vs 4.6 mm [2.9–5.4] in quiescent cases.
Conclusion: Ultrasound localization microscopy allows to visualize microvessels within the carotid arterial wall, with significantly greater MB passage in patients with active Takayasu’s arteritis. ULM provides for the first time a precise visualization in vivo of the vasa vasorum and gives access to quantification of the inflammation of the arterial wall through its vascularity.
lower panel: microbubble tracking data by individual acquisition for each patient. Patients are presented in groups with active (red) and quiescent (blue) Takayasu arteritis.
To cite this abstract in AMA style:
Goudot G, Jimenez A, Mohamedi N, Sitruk j, Khider L, Mortelette H, Papadacci C, Hyafil F, Tanter M, Messas E, Pernot M, Mirault T. Ultrasound Localization Microscopy as a New Tool for Takayasu’s Arteritis Activity Assessment, a Deep Insight Within Carotid Wall Inflammation [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/ultrasound-localization-microscopy-as-a-new-tool-for-takayasus-arteritis-activity-assessment-a-deep-insight-within-carotid-wall-inflammation/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ultrasound-localization-microscopy-as-a-new-tool-for-takayasus-arteritis-activity-assessment-a-deep-insight-within-carotid-wall-inflammation/