Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Abatacept and tocilizumab have been shown to be efficacious for the treatment of rheumatoid arthritis (RA), even in patients refractory to tumor necrosis factor inhibitor (TNFi). However, reports on their long term efficacy in clinical practice are scarce. The aim of this study was to describe two-year drug survival and clinical response in RA patients treated with abatacept or tocilizumab in routine care. It is an extension of previously published 48-week data1, based on data from the nationwide Danish DANBIO registry
Methods:
In the DANBIO registry we identified 230 and 447 RA patients treated with abatacept and tocilizumab, respectively. The clinical efficacy was assessed by drug survival and by changes in DAS28 and EULAR response rates after 48 and 96 weeks. No imputation of missing values was done. No direct comparison of the 2 drugs was made.
Results:
Of the patients receiving abatacept and tocilizumab, respectively, 22%/25% (abatacept/tocilizumab) were male, median (interquartile range, IQR) age 55(45-64)/57(46-65) years, disease duration 5(1-13)/5(1-11) years and number of previous biological drugs 2(2-3)/2(1-3), >99%/>99% of patients, had previously received ≥1 TNFi. Rheumatoid factor was positive in 79% and 77% of patients with available data (143/230 and 290/447), respectively.
After 48 and 96 weeks, 54%/66% and 39%/58% of patients treated with abatacept/tocilizumab were still receiving the drug, respectively.
Among patients with available response data, median DAS28 was in the abatacept group 5.2, 3.2 and 2.9 at baseline, week 48 and week 96, respectively, while 5.3, 2.7 and 3.0 in the tocilizumab group.
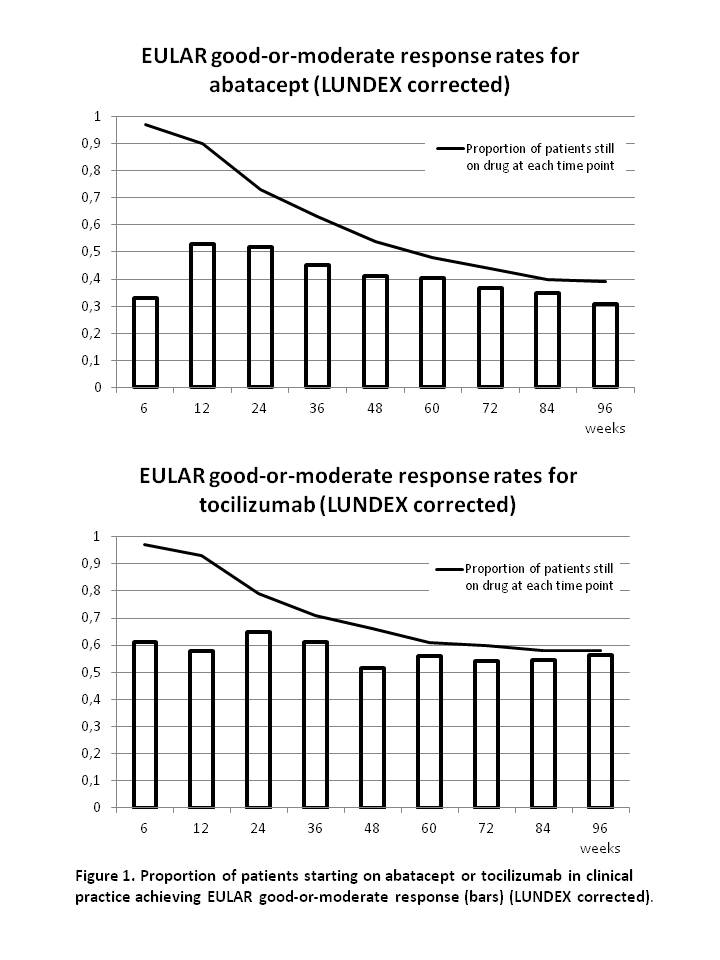
At week 48 and 96, the remission rates for abatacept/tocilizumab were 29%/49% and 38%/41%, respectively and rates of good-or-moderate EULAR response was 76%/87% and 79%/97% at week 48 and 96. Response rates after correction for proportion of patients still on drug (LUNDEX values2) are presented in figure 1.
Conclusion:
In RA patients (>99% TNFi failures) treated with abatacept and tocilizumab, 54%-66% of patients were still receiving the drug after 48 weeks, and 39%-58% after 96 weeks. Due to the non-randomised study design, no direct comparison of the drugs were made. Both drugs significantly decreased the disease activity, and a good-or-moderate EULAR response was seen in the majority (76%-87%) of patients after 48 weeks (87%-97% after 96 weeks). After correction for patients who had withdrawn, response rates were lower. This stresses the importance of transparency in the reporting of observational data.
Reference List
1. Leffers HC, Ostergaard M, Glintborg B et al. Efficacy of abatacept and tocilizumab in patients with rheumatoid arthritis treated in clinical practice: results from the nationwide Danish DANBIO registry. Ann Rheum Dis 2011;70(7):1216-1222.
2. Kristensen LE, Saxne T, Geborek P. The LUNDEX, a new index of drug efficacy in clinical practice: results of a five-year observational study of treatment with infliximab and etanercept among rheumatoid arthritis patients in southern Sweden. Arthritis Rheum 2006;54(2):600-606.
Disclosure:
H. Leffers,
None;
M. Østergaard,
Abbott Immunology Pharmaceuticals,
2,
Abbott, Centocor, Merck, Pfizer. Roche, UCB,
5,
Abbott, Merck, Mundipharma, Novo, Pfizer, UCB,
8;
B. Glintborg,
None;
N. S. Krogh,
None;
U. Tarp,
None;
T. Lorenzen,
Roche, Pfizer,
6;
A. Hansen,
MSD,
5;
M. S. Hansen,
Abbott, Roche, UCB,
5,
Abbott, Roche, UCB,
6;
L. Dreyer,
None;
M. S. Jakobsen,
None;
M. L. Hetland,
Roche Pharmaceuticals,
5,
MSD, BMS, UCB, Abbott, Pfizer,
8.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/two-year-drug-survival-and-treatment-effect-of-abatacept-and-tocilizumab-in-the-treatment-of-rheumatoid-arthritis-in-routine-care-results-from-the-nationwide-danish-danbio-registry/