Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Lupus nephritis (LuN) causes significant morbidity and mortality, but predicting which patients will progress still remains imprecise. Current classification schema for LuN and its treatment are based exclusively or primarily on the glomerulus. Multiple studies have found that such classification schemes inconsistently predict outcomes, whereas tubulointerstitial inflammation (TII) has been shown to associate with poor renal survival. However, long-term data from a cohort with mostly African American (AA) patients with severe TII are still lacking. We aimed to determine the association between TII and long-term renal survival in LuN, and at-biopsy factors associated with moderate to severe TII.
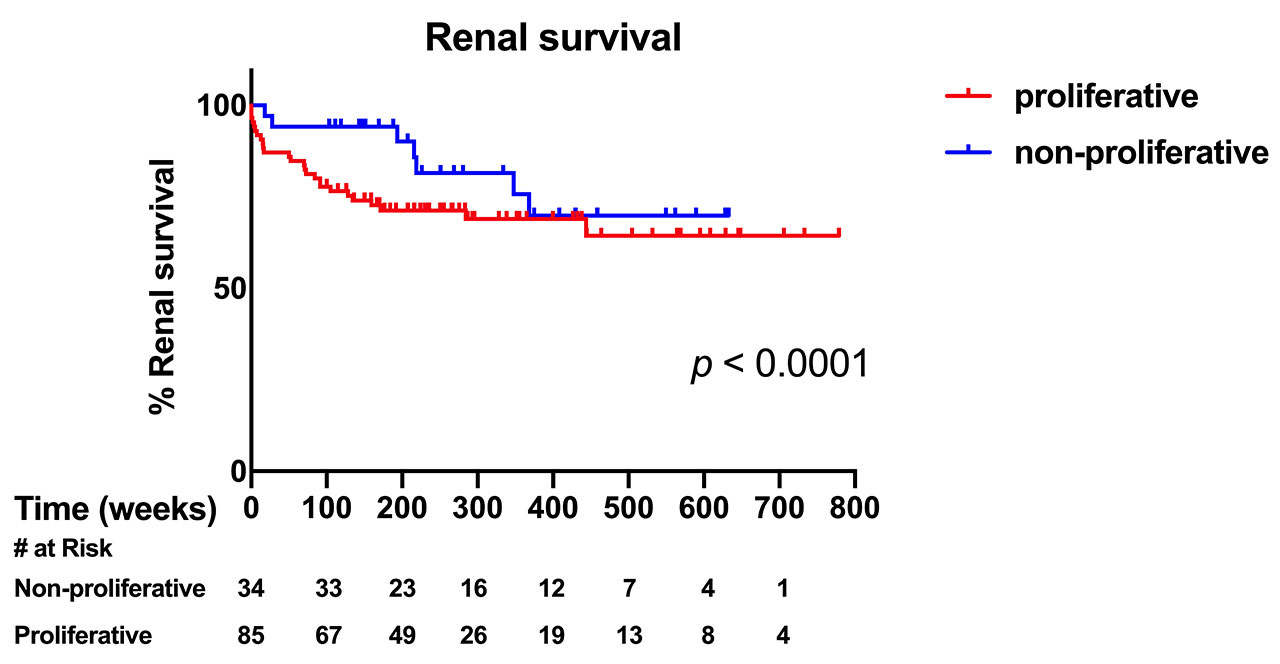
Methods: Retrospective data from LuN subjects who had native kidney biopsies done from 2003 through 2014 were collected. Only those with at least 2 years of follow-up from the time of biopsy were included for analysis. Subjects were classified by International Society of Nephrology/Renal Pathology Society (ISN/RPS) criteria, and Class III and IV cases were combined into a proliferative class for analysis. TII was scored semi-quantitatively through light and immunofluorescence (CD45) microscopy by a blinded pathologist, and given scores from 0 – 3: 0 (< 10% of involvement, minimal), 1 (10 – 25%, mild), 2 (26 – 50%, moderate) and 3 ( >50%, severe). Bivariate comparisons and multivariate logistic regression (MLR) analysis were performed to determine at-biopsy factors associated with moderate to severe TII. Renal survival analyses were done though Kaplan – Meier technique with time to end-stage renal disease (ESRD) with curves compared through the log-rank test.
Results: Among 122 subjects, 75.4% were AA, 84.4% were female, and 73.0% had proliferative LuN. The median follow-up period was 5.3 years (interquartile range 3.4 – 8.4 years). 60 subjects had moderate to severe TII, and they had higher percent of AA (91.7 vs 59.7%, p < 0.0001), higher median creatinine (1.5 vs 0.7 mg/dL, p < 0.0001), higher degree of proteinuria (3.8 g/day vs 1.8 g/day, p < 0.0001), and higher glomerular activity index (p = 0.02) and chronicity index (CI, both glomerular [p = 0.0001] and tubulointerstitial [p < 0.0001]) than those with minimal to mild TII. MLR analysis showed that moderate to severe TII was only associated with AA ethnicity (Odds Ratio [OR] 5.38, p = 0.028) and tubulointerstitial CI (OR 3.85, p = 0.001) but not with proliferative class or glomerular CI. Renal survival analysis found that subjects with moderate to severe TII had worse renal survival (approximately 50% with ESRD by 4th year) compared to those with minimal to mild TII (hazard ratio 5.01, p < 0.0001). There was no renal survival difference based on the presence of proliferative LuN (p = 0.2).
Conclusion: Higher degree of TII predicted worse renal survival, whereas ISN/RPS classification was not prognostic. Only AA ethnicity and tubulointerstitial CI were associated with moderate to severe TII at biopsy.
To cite this abstract in AMA style:
Oshinsky C, Siddiqui M, Liarski V, Chang A, Clark M, Ko K. Tubulointerstitial Inflammation Predicts Outcomes in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/tubulointerstitial-inflammation-predicts-outcomes-in-lupus-nephritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tubulointerstitial-inflammation-predicts-outcomes-in-lupus-nephritis/