Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Polymyalgia rheumatica (PMR) treatment is predominantly based on long-term corticosteroids, which results in significant corticosteroid-related toxicities. Studies1,2 have shown patients with PMR are exposed to years of corticosteroid treatment. Therefore, we aimed to ascertain the duration of steroid treatment in a cohort of PMR patients at an academic medical center and establish the success rate in discontinuing steroid treatment at years one and two after the initiation of the treatment.
Methods: A retrospective observational study was done using the data collected from the rheumatology clinic at an academic Medical Center. We reviewed 323 charts with a diagnosis of PMR from 2015-to 2019, and 121 patients met the inclusion criteria for the study. Patients with a primary diagnosis of PMR without any other rheumatologic conditions and a minimum of 2-year follow-up since diagnoses were included in this study. Patients with PMR diagnosis and any other rheumatologic illnesses and on any other therapy except for prednisone were excluded.
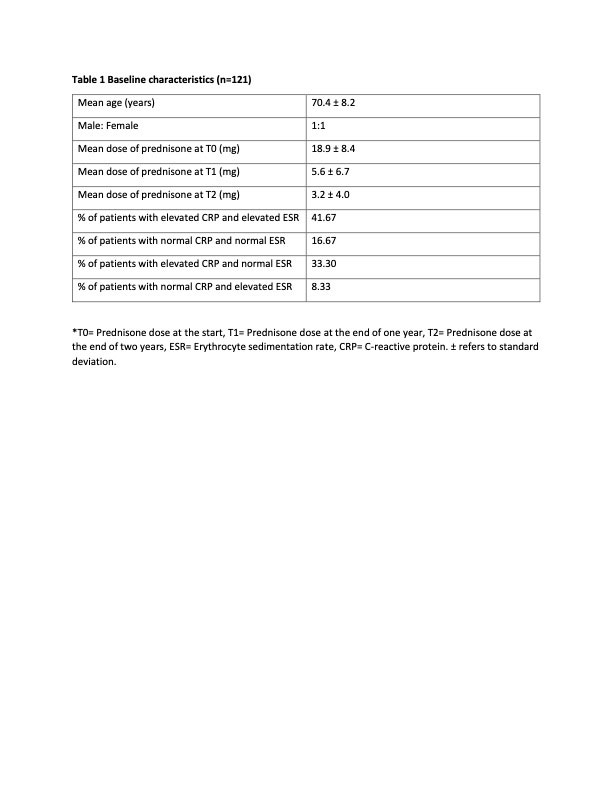
Results: The mean age of the patient population was 70 years, and the gender distribution was approximately 1:1, with 58 females and 63 males. The mean prednisone dose at the beginning (T0) was 18.9 mg daily, at the end of one year (T1) 5.6 mg, and at the end of two years (T2) 3.2 mg daily. 17.4% of patients were off prednisone at the end of one year, and only 24% were off prednisone at the end of two years. 3.3% of patients relapsed and had to go back on corticosteroid treatment. The majority of the patients had elevated markers of inflammation [ESR (Erythrocyte sedimentation rate) or CRP (C-reactive protein)], with only 16.67% of patients having normal values on presentation.
Conclusion: The clinical course of polymyalgia rheumatica is associated with significant corticosteroid dosing over the years, and the success rate achieved in getting patients off of prednisone is dismal. Limitations of this study include its retrospective nature and the possibility of selection bias as we only included patients with two years of follow-up. The results, however, reinforce the need for further studies to identify and induct an alternative disease modification anti-rheumatic drug (DMARD) in the treatment regimen of PMR.
To cite this abstract in AMA style:
Tiwari V, Devalla V, Campbell E, Rigby W. Trends in the Cumulative Exposure to Corticosteroids in Polymyalgia Rheumatica (PMR) Patients: A Single Academic Center Experience [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/trends-in-the-cumulative-exposure-to-corticosteroids-in-polymyalgia-rheumatica-pmr-patients-a-single-academic-center-experience/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-the-cumulative-exposure-to-corticosteroids-in-polymyalgia-rheumatica-pmr-patients-a-single-academic-center-experience/