Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cutaneous lupus erythematosus (CLE) is a heterogeneous chronic disease with potential for long lasting morbidity. Studies that provide incidence data on the entire spectrum of CLE are needed to better estimate the disease burden. Furthermore, it is unclear whether secular changes in risk factors such as smoking over the decades have had an impact in CLE incidence. We aimed to investigate the incidence of CLE and its secular trends from 1976 to 2018.
Methods: All patients in a geographically well-defined area who received a SLE or CLE diagnostic codes or the following laboratory measures: ANA, anti-double stranded DNA, anti-Sm, complement, and antiphospholipid antibodies underwent a thorough review of clinical notes, pathology and medical photography.
Incident cases were defined based on the criteria by Sontheimer. We categorized CLE as follows: discoid lupus erythematosus (DLE), lupus panniculitis (LP), lupus tumidus (TL), chilblain lupus (CHLE) and subacute cutaneous lupus (SCLE). Those with uncertain diagnosis or subtype were reviewed by a CLE expert dermatologist. The incidence date was when the skin lesion was first described in the medical record. We included both patients with CLE as well as those with systemic lupus erythematosus (SLE) with cutaneous manifestations. We considered chronic CLE in patients who did not have a concurrent (within one year of cutaneous manifestations) or previous diagnosis of SLE.
Age and sex specific incidence rates were adjusted to the 2010 US white population. The 95% confidence intervals for incidence rates were computed assuming that the data follows a Poisson distribution.
Results: We identified a cohort of 209 incident CLE cases between 1976 and 2018. Mean age was 50.3 (SD 17.2). 72% were female. The racial make-up was 5% Asian, 7% Black, 87% Caucasian, 1% Native American. 2% percent were Hispanic. The proportion of Caucasians decreased over the years.
Out of 209 patients, 13 (6.2%) had a previous or concurrent diagnosis of SLE by the ACR 97 criteria and 94% were considered chronic CLE.
The distribution of the CLE subtypes was: 23% SCLE, 63% DLE, 1% LP, 3% CHLE, 7% TL. 1% of the cases had more than one subtype. The proportion of LT, CHLE and LP increased over the decades. (Table 1)
The overall incidence rate of CLE between 1976 and 2018 was 4.5 (95%CI: 3.9, 5.2) per 100,000. Females had a higher incidence than males: 6.2 (95%CI: 5.2, 7.2) and 2.7 (95%CI: 2.0, 3.5) per 100,000, respectively. Age- and sex-specific incidence rates peak at the 60-69 age group in both females and males, 11.8 and 5.6 per 100,000, respectively. (Table 2) There was an increase in CLE incidence during 1985-1995 that was observed in both sexes and posteriorly trended downwards. (Figure 1)
Conclusion: Our data shows that the overall incidence of CLE has remained stable over the decades with a sudden increase in 1985-1995 with posterior return to prior rates. The majority of the CLE cases do not have SLE prior or concurrent to diagnosis. The clinical characteristics of CLE changed with rising proportion of TL, SCLE, CL, LP cases. More studies are needed to investigate whether these changes are due to rising awareness of rare subtypes or changes in environmental or demographic factors.
 Table 1. Demographics and Clinical Characteristics of Cutaneous Lupus Erythematosus
Table 1. Demographics and Clinical Characteristics of Cutaneous Lupus Erythematosus
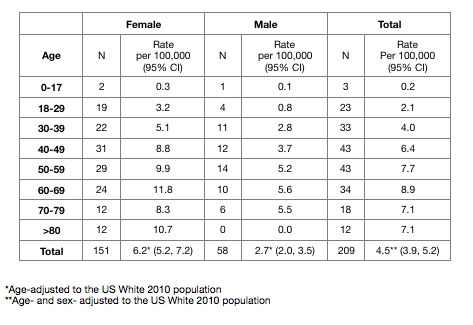 Table 2. Age- and sex-specific incidence rates for CLE
Table 2. Age- and sex-specific incidence rates for CLE
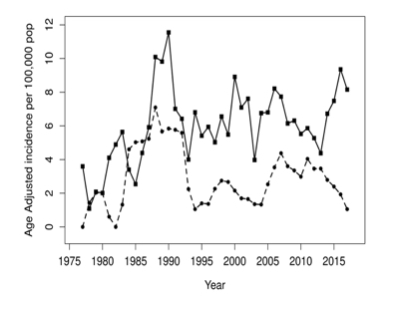 Figure 1. Trends in age-adjusted Cutaneous Lupus Erythematosus incidence over time by Sex (female is solid line and male is dashed line)
Figure 1. Trends in age-adjusted Cutaneous Lupus Erythematosus incidence over time by Sex (female is solid line and male is dashed line)
To cite this abstract in AMA style:
Hocaoglu M, Davis M, Osei-Onomah S, Dabit J, Giblon R, O'Byrne T, Crowson C, Duarte-Garcia A. Trends in Incidence of Cutaneous Lupus Erythematosus from 1976 to 2018: A Population-Based Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/trends-in-incidence-of-cutaneous-lupus-erythematosus-from-1976-to-2018-a-population-based-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-incidence-of-cutaneous-lupus-erythematosus-from-1976-to-2018-a-population-based-study/
