Session Information
Date: Monday, November 8, 2021
Title: Abstracts: Reproductive Issues in Rheumatic Disorders (1464–1467)
Session Type: Abstract Session
Session Time: 4:15PM-4:30PM
Background/Purpose: Autoimmune connective tissue diseases disproportionately affect women of childbearing age. Systemic sclerosis (SSc) is associated with increased risk of adverse pregnancy outcomes (APO). However, changes in obstetric practices may have improved SSc pregnancy outcomes in recent years, as seen for SLE. We sought to examine APO occurrences among women with and without SSc and determine whether APOs have declined over the past 18 years in a large nationwide sample.
Methods: The National Inpatient Sample (NIS) database for years 2000–2017 was used to derive national estimates of delivery-associated hospitalizations. SSc deliveries were identified using ICD codes, excluding those with concurrent SLE or RA. Each SSc hospitalization was matched by age, delivery year, and race to non-SSc hospitalizations from the NIS in a 1:100 ratio. APOs included fetal death, Cesarean delivery, hospital length of stay, preterm birth, intrauterine growth restriction, and hypertensive disorders of pregnancy (preeclampsia, eclampsia, gestational hypertension, and superimposed preeclampsia). All analyses accounted for the complex survey design and sampling weights were applied. Adjusted odds ratios for each APO for the entire study period were calculated from multivariable regression analyses using maternal age, race, diabetes mellitus, and preexisting hypertension as covariates. To compare differences in temporal trends in APOs between SSc and non-SSc deliveries, we pooled data into 6-year intervals and applied logistic or linear regression with an interaction term between SSc (yes vs. no) and year.
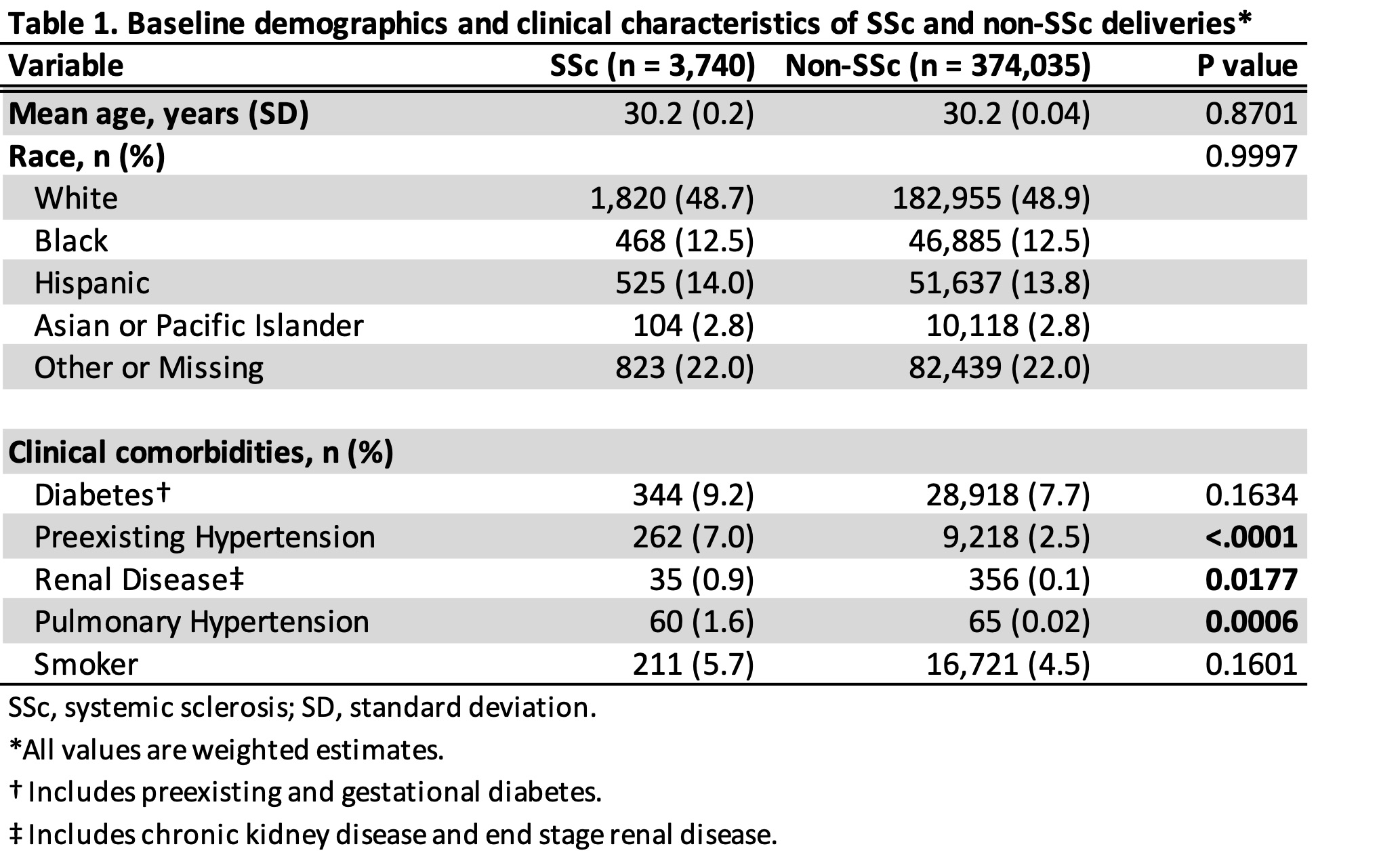
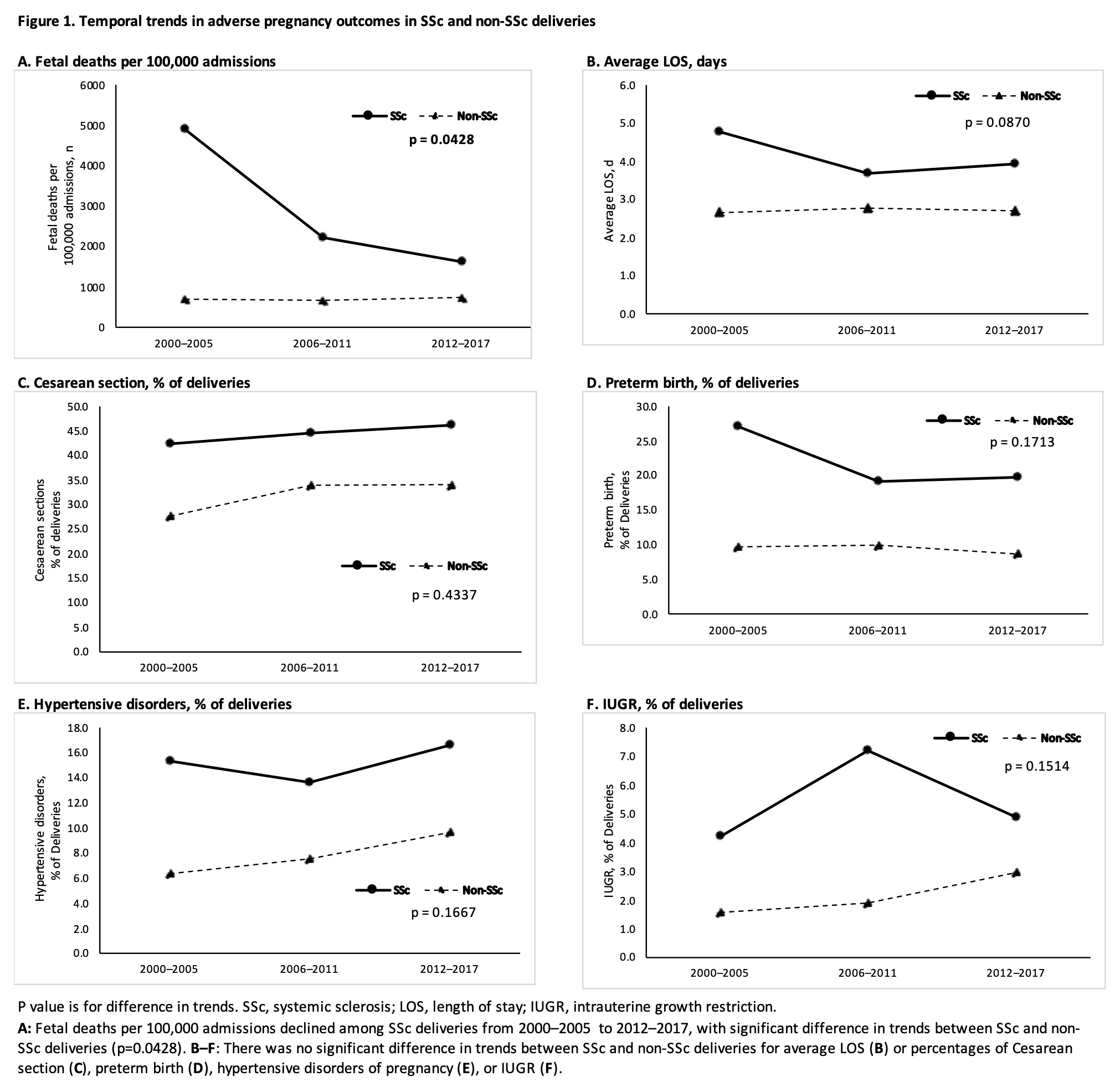
Results: From 2000 to 2017, there were 3,740 (95% CI 3,446–4,034) delivery-associated hospitalizations for women with SSc. Mean maternal age at delivery was 30 years. There were significant differences in comorbidities between the SSc and non-SSc groups including pre-existing hypertension, renal disease, and pulmonary hypertension (Table 1). The odds of all APOs during the entire study period were significantly higher in SSc vs. non-SSc deliveries (Table 2). Fetal deaths notably declined in SSc deliveries from 4,896 per 100,000 delivery-related admissions in 2000–2005 to 1,619 per 100,000 in 2012–2017. Difference in trend over time for fetal death was significant (p=0.043) between SSc and non-SSc deliveries, but trends in other APOs were not significantly different (Figure 1).
Conclusion: In this large nationwide sample, the risk of fetal death among women with SSc markedly improved over the past 18 years. We focused on delivery-associated hospitalizations rather than all obstetric hospitalizations; therefore, fetal death represents stillbirth, and captures neither miscarriages earlier in pregnancy nor neonatal death. The risk of other APOs remained high in SSc deliveries, and further studies are needed to determine what factors or therapeutics can improve these outcomes.
To cite this abstract in AMA style:
Kawano Y, Kolstad K, Li S, Simard J, Chung L. Trends in Adverse Pregnancy Outcomes Among Women with Systemic Sclerosis in the United States [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/trends-in-adverse-pregnancy-outcomes-among-women-with-systemic-sclerosis-in-the-united-states/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-adverse-pregnancy-outcomes-among-women-with-systemic-sclerosis-in-the-united-states/