Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is treated with glucocorticoids, anti-malarials, immunosuppressive medications, and, more recently, biologics (specifically, belimumab and rituximab). While belimumab had positive results in trials, the rituximab trials were negative. With expanding therapeutic options, it is important to understand the current utilization patterns among patients with SLE, as this knowledge can inform policy, formulary planning and future needs. Little is known about the population level trends in the use of these agents, particularly during the early-years of the disease. We described the trends in medication use during the first five years after SLE diagnosis.
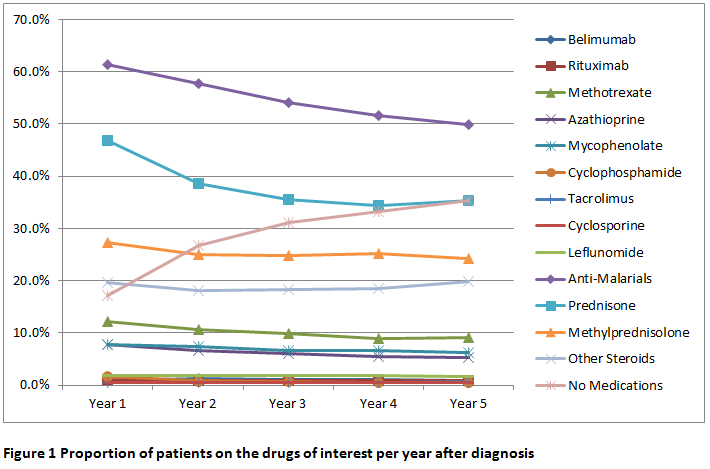
Methods: Using a large administrative database of commercially insured and Medicare Advantage beneficiaries across the U.S. (OptumLabs Data Warehouse) from 2006-2016, we identified newly diagnosed patients with SLE (ascertained using three ICD-9/10 codes separated by ≥30 days). Patients had at least two years of enrollment prior to SLE diagnosis and were followed for a maximum of five years after diagnosis or until disenrollment, whichever happened first. Follow up was calculated using the person-years method. For every year after diagnosis, we estimated the proportion of patients who filled prescriptions for the drugs of interest (figure).
Results: We identified 10,274 patients with newly diagnosed SLE, of whom 4227 had ≥5 years of follow up. Mean age at diagnosis (SD) was 45.7 (12.1)years, 89% were female, 62% were White, 17% Black, 12% Hispanic, 4% Asian, and 5% other/unknown race. Anti-malarials were the most frequently used drugs, filled at least once by 61% of patients during the first year after diagnosis, and decreased to 50% at five years after diagnosis. Prednisone was the second most frequently used drug, used by 47% of patients during the first year of the disease and 35% at 5 years after diagnosis. Methylprednisolone and other steroids were used by 20% or more patients consistently during the 5 years of follow up. Methotrexate was used by 12% of the patients during the first year, and was most common immunosuppressive drug prescribed. Azathioprine and mycophenolate mofetil were each used by 8% of the patients. Rituximab was used by 1% and belimumab by 2% of patients consistently during the five years of follow up. Overall there was a progressive decline in the use of most medications. By year five, 35% of the SLE patients did not fill prescriptions for any of the drugs of interest.
Conclusion: During the first five years after SLE diagnosis, there was a progressive decline in the use of all immunosuppressive medications. Five years after diagnosis, a high proportion of patients with SLE continue receiving glucocorticoids. Is unclear if these observations are due to lower disease activity over time, medication intolerance, increased noncompliance or combination thereof.
To cite this abstract in AMA style:
Duarte-Garcia A, Crowson CS, McCoy R, Schilz S, Van Houten H, Sangaralingham L, Chowdhary VR, Amin S, Warrington KJ, Matteson EL, Shah N. Treatment Trends of Systemic Lupus Erythematosus during Early-Years of the Disease [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/treatment-trends-of-systemic-lupus-erythematosus-during-early-years-of-the-disease/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-trends-of-systemic-lupus-erythematosus-during-early-years-of-the-disease/