Session Information
Date: Monday, November 13, 2023
Title: (1365–1382) Sjögren’s Syndrome – Basic & Clinical Science Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Currently, no systemic therapies have been approved for Sjögren’s disease (SjD) due to limited evidence regarding efficacy. However, biologics are often used in patients with active systemic involvement. Real-world data on treatment patterns and off-label use of biologics in SjD are lacking. We aimed to describe treatment patterns and identify potential drivers of biologic prescription in patients with primary SjD in real-world clinical settings.
Methods: Data were drawn from the Adelphi SjD Disease Specific Programme™, a cross-sectional survey of rheumatologists and their consulting patients with SjD in France, Germany, Italy, Spain, and the United States of America from 2018. Rheumatologists completed patient record forms for their next six SjD patients, reporting on demographics, clinical characteristics, physician-perceived disease severity (mild, moderate, severe), treatment history and reasons for treatment selection. A least absolute shrinkage and selection operator (LASSO) regression model was applied to identify drivers associated with biologic prescription. All other data were analyzed descriptively.
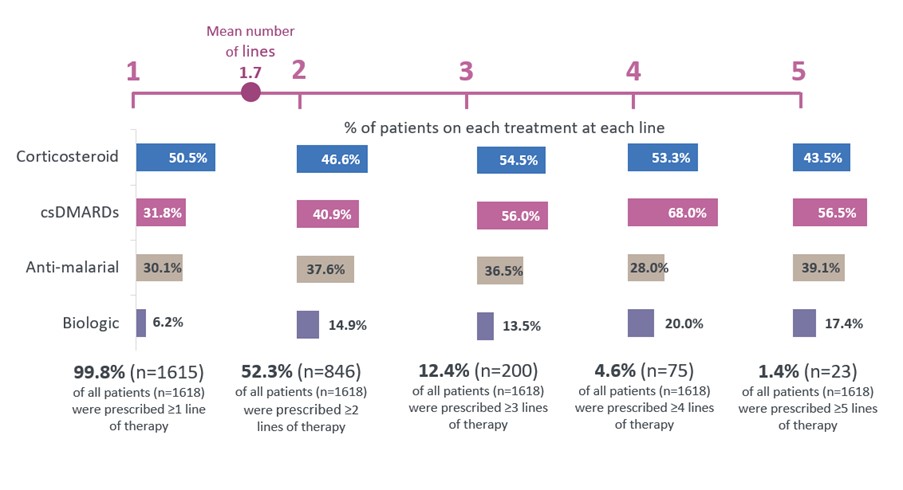
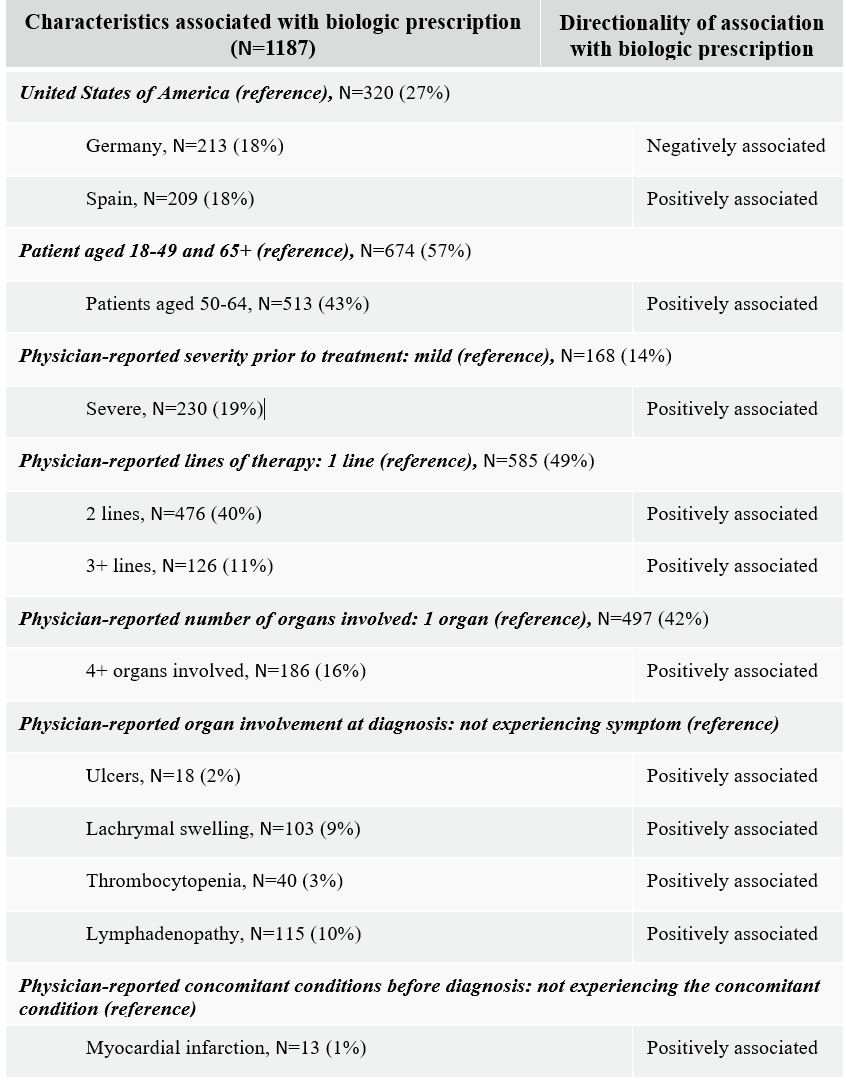
Results: 316 rheumatologists reported data for 1879 patients with SjD; 89% of patients were female, the mean (SD) age was 53 (12.18) years, 89% of patients were white and 67% of patients had moderate SjD as perceived by rheumatologists prior to SjD treatment. Of 1618 patients with complete data on treatment patterns, 99.8% (N=1615) of patients received ≥1 line of therapy (LoT), 52% (N=846) of patients received ≥2 LoTs and 12% (N=200) of patients received ≥3 LoTs. Corticosteroids were prescribed in 44-55% of patients with SjD, while biologics were least prescribed (6-20%) and were typically initiated at LoT 2 or later (Figure 1). LASSO regression (N=1187) revealed a higher likelihood of biologic prescription at 2 or later LoT. Patients with physician-perceived severe disease were also more likely to be prescribed a biologic than those with mild disease, as were patients with ≥4 organs involved at diagnosis (Table 1).
Rheumatologists’ top five reasons for biologic prescription (N=223) included efficacy in treating organ manifestations (55%), reducing pain (51%), intent to slow disease progression (51%), and maintaining quality of life (50%). A further 49% also reported wanting to reduce steroid burden, even though around 50% of patients with biologic prescriptions had concomitant steroid use.
Conclusion: From this international survey, we found that patients with more LoTs, physician-perceived severe primary SjD, and greater organ involvement were more likely to be prescribed biologics. Across all LOTs, biologic use was low reflecting the lack of approved or effective drugs in SjD. Overall corticosteroid use was common, suggesting that available biologics may not be efficacious enough to reduce steroid use in SjD. There remains an unmet need among patients with primary SjD and further research is warranted to fully understand the impact of biologics on corticosteroid use among patients with SjD.
Progression in line of therapy defined as change in treatment regimen (including addition or removal of any other class of therapy from a regimen). Overall, 1618 patients had complete treatment pattern data. At each line of therapy, the % of patients prescribed each treatment class does not sum to 100% due to concomitant treatment class prescription. csDMARDs (conventional synthetic disease-modifying anti-rheumatic drugs) include azathioprine, methotrexate, cyclosporine, cyclophosphamide, mycophenolate mofetil and other csDMARD. Anti-malarial includes hydroxychloroquine and other anti-malarials.
Note that base size differs from main sample due to data completeness for all variables.
To cite this abstract in AMA style:
McCoy S, Baer A, Xi A, Castellano G, Barton V, Amatucci A, Alevizos I, Patel H. Treatment Patterns and Drivers of Biologic Prescriptions in Patients with Primary Sjögren’s Disease: Results from a Multinational, Real-World Survey [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/treatment-patterns-and-drivers-of-biologic-prescriptions-in-patients-with-primary-sjogrens-disease-results-from-a-multinational-real-world-survey/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-patterns-and-drivers-of-biologic-prescriptions-in-patients-with-primary-sjogrens-disease-results-from-a-multinational-real-world-survey/