Session Information
Date: Sunday, November 5, 2017
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Crude prevalence estimates indicate Down syndrome arthropathy (DA) is 3-8 times more common than juvenile idiopathic arthritis (JIA), however, DA is still largely under recognized, and has a 2 year average delay from onset of symptoms to diagnosis. The majority of patients with DA present with greater than 5 affected joints, with small joints affected more predominantly. Additionally, treatment can be challenged by lack of efficacy and intolerance. Further, gaps in literature exist around optimal treatment approach and outcomes. The objective of this study was to investigate treatment approach and outcomes of DA at our institution.
Methods: In a retrospective chart review, potential DA patients were identified through electronic medical record system (EMR) from January 1, 1995 to December 31, 2015. ICD-9-CM codes were used to identify patients (less than 18 years of age) with both Down Syndrome (DS; 758.0) and JIA (714.3, 714.31, 714.32, 714.33). Individual charts were then manually reviewed to confirm diagnosis of DS and JIA. Chart review included analysis of all documents found in the EMR, including clinical visits and treatment data.
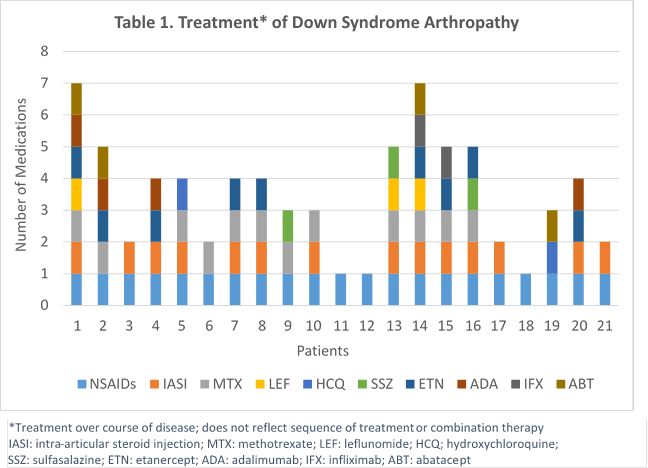
Results: Of 26 identified patients, (3 did not have DS and 2 had incomplete records) 21 met inclusion criteria and were analyzed. Patients were 62% female with polyarticular, RF negative presentation at diagnosis and had a mean (SD) follow-up of 4 (±4) years. There was a 19 month (±16) mean delay in diagnosis of arthritis from symptom onset, and at diagnosis of arthritis, 71% had morning stiffness with an average of 14 (±10) active joints, 12 (±10) limited joints, and mean physician global of disease activity (MD PGA) of 4.9 (±2). All patients were started on nonsteroidal anti-inflammatory drugs (NSAIDs) at diagnosis with 33% simultaneously starting a disease modifying antirheumatic drug (DMARD), and 5 % a Biologic. Over the course of disease, 62% used a DMARD (57% MTX) and 48% used a biologic (90% etanercept). Six patients (29%) had at least one change in DMARD and another six patients had at least one change in biologic therapy (Table 1). Compared to diagnosis, at the last recorded visit there was a significant decrease in mean (SD) active joints: 3 (± 4), limited joints: 5 (± 6) and MD PGA: 1.7 (± 1.6) (p<0.01 respectively). Of those on DMARD therapy 54% had drug discontinuation due to side effects and 56% had an inadequate response to first-line biologic therapy.
Conclusion: Down syndrome arthropathy remains under recognized despite reports of higher prevalence compared with JIA. Although treatment approach is unclear, DA patients have significant improvement in the number of active and limited joints with NSAID, DMARD, and biologic therapies. Other barriers that inhibit optimal treatment and outcomes are DMARD toxicity and lack of anti-TNF effectiveness. More research is needed to determine the timing and choice of optimal therapy in patients with Down syndrome.
To cite this abstract in AMA style:
Jones JT, Danawala L, Talib N, Becker ML. Treatment Outcomes of Down Syndrome Arthropathy [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/treatment-outcomes-of-down-syndrome-arthropathy/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-outcomes-of-down-syndrome-arthropathy/