Session Information
Date: Saturday, November 12, 2022
Title: Health Services Research Poster I: Lupus, RA, Spondyloarthritis and More
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Most patients with undiagnosed ankylosing spondylitis (AS) seek care for back pain from primary care providers (PCPs), and treatment strategies adopted by PCPs may vary from those used by rheumatologists.1 The objective of this analysis was to examine the prescribing habits of rheumatologists and PCPs who were treating patients with AS.
Methods: A retrospective cross-sectional study was performed using electronic medical records from the health systems of the University of Pennsylvania (UPENN), the University of Utah (Utah), and from MetroHealth. Patients who were diagnosed with AS (International Classification of Diseases, 10th Revision code M45.X or M08.1) between January 2017 and September 2020 were included. Baseline characteristics at the time of first diagnosis code, visits to rheumatologists and PCPs, and prescribed therapies are reported descriptively.
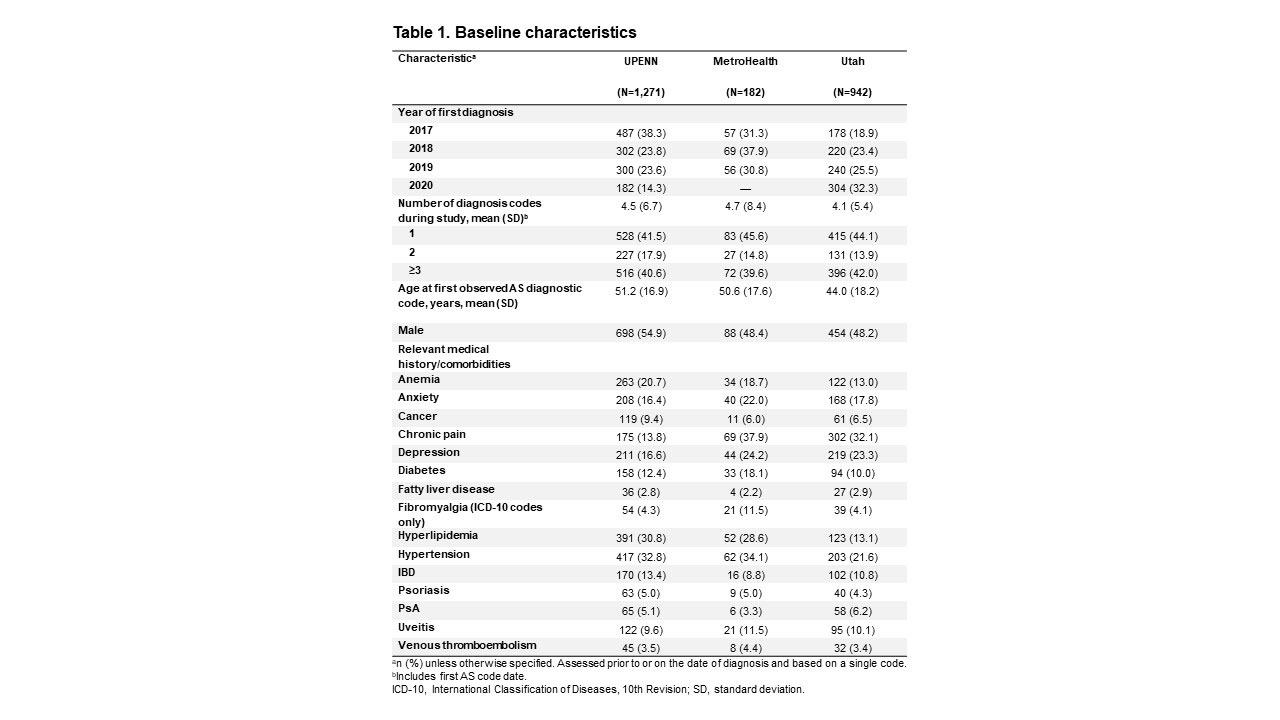
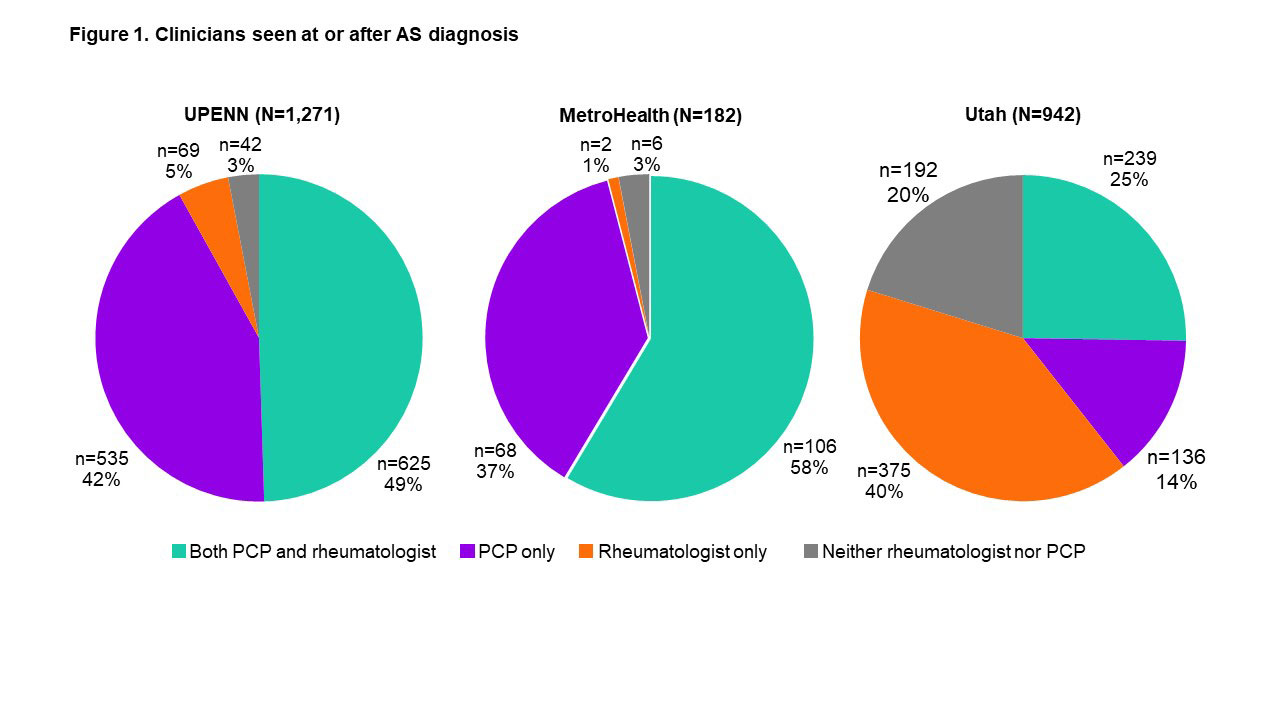
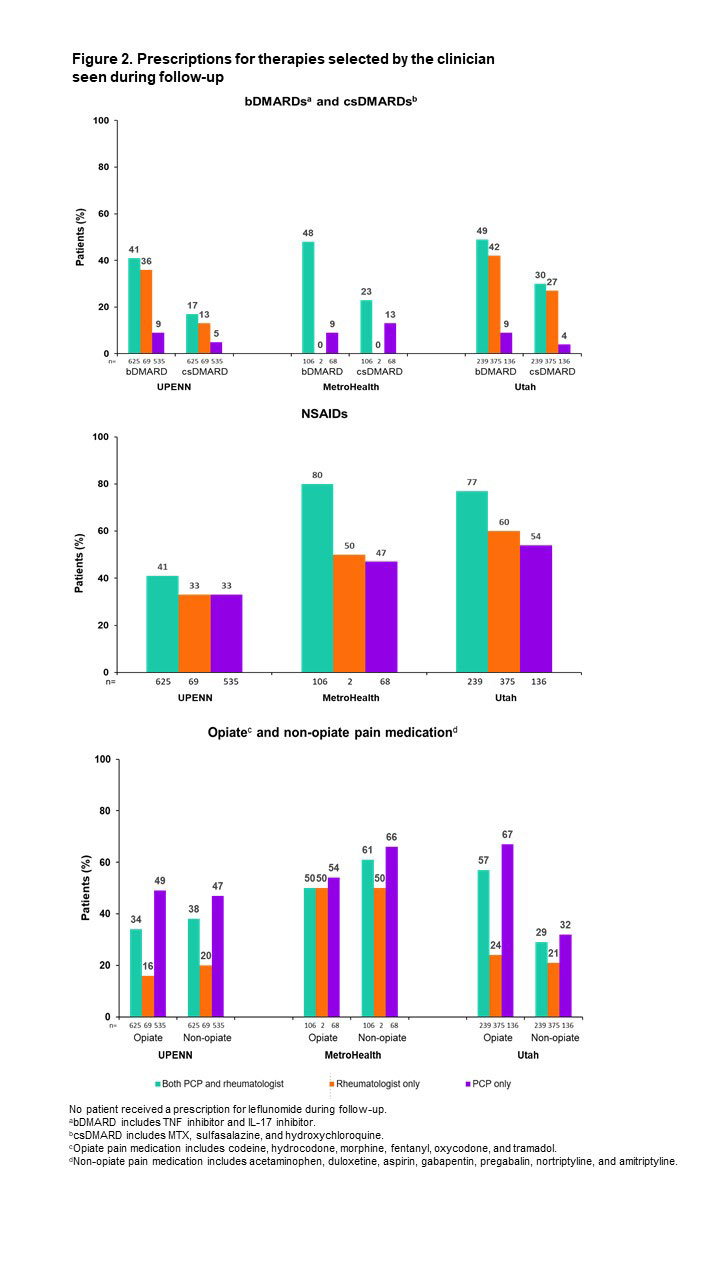
Results: In total, 2,395 patients with a qualifying diagnosis code were identified: UPENN, n=1,271; MetroHealth, n=182; Utah, n=942. The mean age of patients was 51 years in UPENN and MetroHealth systems, and 44 years in the Utah system; 55%, 48%, and 48% of patients in the UPENN, MetroHealth and Utah systems, respectively, were male (Table 1). Common comorbidities included anemia, anxiety, depression, hyperlipidemia, and hypertension, although prevalence differed by health system. In contrast, the prevalence of inflammatory bowel disease, uveitis, and psoriasis were generally consistent across the three health systems. The proportions of patients who were seen by a rheumatologist, a PCP, or both, also differed by health system (Figure 1). Across all institutions, patients followed by a rheumatologist were far more likely to receive biologic DMARD (bDMARD) prescriptions than those followed by a PCP alone (Figure 2). Overall, conventional synthetic DMARDs (csDMARDs) were prescribed less frequently than bDMARDs and were not commonly prescribed to patients who were followed up by PCPs alone. Both opiate and non-opiate pain medications were commonly used and were most frequently prescribed to patients, followed up by PCPs alone.
Conclusion: In this population of patients with AS followed in three different health systems, bDMARDs and csDMARDs were more frequently prescribed to patients seen by a rheumatologist than to patients seen by a PCP alone. By contrast, opiate and non-opiate pain medications were prescribed more frequently to patients who were followed up by a PCP alone. These findings from multiple institutions demonstrate the variability in prescribing patterns between PCPs and rheumatologists and highlight areas for targeted education of clinicians caring for patients with AS.
Reference 1.Deodhar A, et al. Clin Rheumatol 2016;35:1769–76
To cite this abstract in AMA style:
Ogdie A, Magrey M, Fitzsimmons R, Abdollahi S, Yong W, Tarabichi Y, Biljan A, Saffore C, Tacelosky K, Walsh J. Treatment of Ankylosing Spondylitis by Primary Care Physicians and Rheumatologists: A Retrospective Study in Three Health Systems [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/treatment-of-ankylosing-spondylitis-by-primary-care-physicians-and-rheumatologists-a-retrospective-study-in-three-health-systems/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-of-ankylosing-spondylitis-by-primary-care-physicians-and-rheumatologists-a-retrospective-study-in-three-health-systems/