Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Even among young women with systemic lupus erythematosus (SLE), accelerated atherosclerosis and coronary artery disease are common complications. Traditional risk scoring methods underestimate cardiovascular (CV) risk in patients with SLE, highlighting the need to account for both traditional and lupus-specific risk factors. Our goal is to evaluate the influence of traditional and lupus-specific risk factors on CV outcomes, and examine potential health disparities in these outcomes, among patients with SLE.
Methods: Data was obtained from an ongoing IRB-approved longitudinal single-center registry of patients with SLE and non-SLE population-matched controls. Demographics, medical / social history, and SLE characteristics (if applicable) was obtained from interviews, exams, and medical record review. Disease damage was determined by SLICC/ACR Damage Index (“any damage” if score ≥1).Descriptive analyses, Pearson’s chi-squared testing, two-sample t-tests, and multivariable logistic regression were performed as appropriate.
Results: 854 patients with SLE and 663 non-SLE population-matched controls were included in our study. Compared to the controls, the risk of myocardial infarction (MI) was higher among SLE patients (OR 10.53, p< 0.01) and risk of stroke was higher among SLE patients (OR 18.55, p< 0.01), adjusted for age, race, and gender.
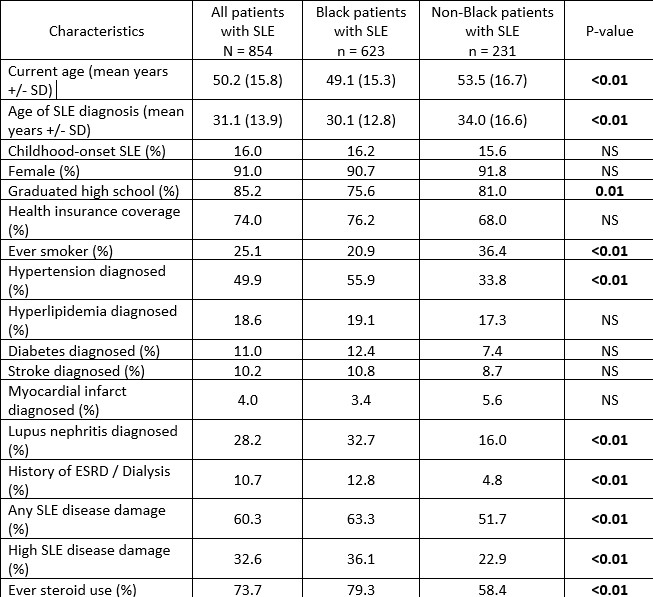
Age of SLE diagnosis and current age were both lower among Black patients compared to non-Black patients (Table 1), with no significant difference in disease duration. Significantly higher rates of hypertension, lupus nephritis (LN), disease damage and steroid use were observed among Black patients, and a higher rate of smoking was observed among non-Black patients. Diabetes, hypertension, and hyperlipidemia were associated with higher risk of stroke and MI in univariate analysis (each p < 0.01). In a multivariate model of the risk among patients with SLE of either a stroke or MI, highest odds were for hypertension (OR 5.24, p< 0.01), adjusted for age, race, gender, education, smoking, hyperlipidemia, diabetes, steroid use, and nephritis.
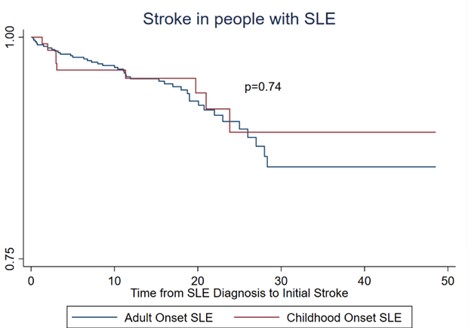
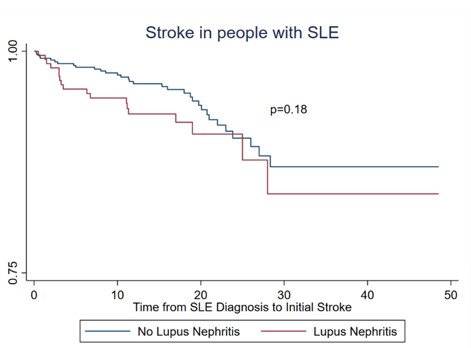
In multivariate regression models those with childhood onset SLE had a similar mean length of time between SLE onset to stroke compared to adult onset SLE (Figure 1), but the stroke age was younger for childhood-onset SLE (23.3 ±10.5 vs 43.3 ±13.8, p< 0.01). Age of MI was also younger for childhood-onset SLE (22.1 ±7.5 vs 47.1 ±11.2, p=0.01). Those with LN had a younger stroke age (32.5 ±14.6 vs 45.0 ±13.5, p< 0.01) and a shorter time to initial stroke compared to those without LN (Figure 2).
Conclusion: We found an increased prevalence of CV indicators and CV outcomes among patients with SLE at a significantly younger age compared to population controls, which is even more striking among patients with childhood onset SLE. Continued racial disparities in several important lupus and CV outcomes were evident, highlighting the need to identify and address care gaps for these high-risk patients. Continued progress in understanding what underlies these outcomes will support needed well-informed clinical interventions in risk factor modification for patients with SLE.
To cite this abstract in AMA style:
Patolia S, Wilson D, Oates J, Kamen D. Traditional and Lupus-Specific Risk Factors for Cardiovascular Events Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/traditional-and-lupus-specific-risk-factors-for-cardiovascular-events-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/traditional-and-lupus-specific-risk-factors-for-cardiovascular-events-among-patients-with-systemic-lupus-erythematosus/