Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The course of childhood-onset Systemic Lupus Erythematosus (cSLE) commonly includes neurocognitive dysfunction, a manifestation with poor prognosis. It has been challenging to diagnose and categorize CNS involvement in cSLE due to its heterogeneity, especially in early stages. As part of development of a comprehensive patient-centered care approach, we are collecting clinical MRI in cSLE patients, including specialized protocols for CNS lupus assessment. Here, we focus on whole-brain volumetric measures from our protocol. We have previously identified multiple areas of gray matter (GM) loss on structural MRI in cSLE patients with neurocognitive deficits. This work is part of our overall aim to identify clinical neuroimaging signatures for patient-specific categorization of CNS involvement and to allow tracking of disease course and treatment response.
Methods: The first 12 cSLE patients referred for a specialized clinical lupus MRI evaluation were analyzed. Appended to a routine clinical brain MRI protocol were sequences for diffusion-weighted imaging, resting-state functional MRI, and so-called synthetic MRI (synMRI). Using multiple weightings, synMRI provides quantitative mapping of tissue magnetic relaxation properties permitting segmentation of gray matter (GM), white matter (WM), cerebrospinal fluid, and myelin tissue classes. Our initial analyses focused on whole-brain volumes, specifically tissue class volumes as percentage of total intracranial volume (%ICV). We assessed the association of GM, WM, myelin, and parenchyma (GM+WM) as %ICV with SLE severity (SLEDAI) and neurocognitive performance via the Pediatric Automated Neuropsychological Assessment Metrics (PedANAM), principle component (PCA) and Multiscore summary scores.
Results: The 12 cSLE patients included 10 females and 4 African Americans, with mean age 16.6 ± 3.1 years. Mean SLEDAI score at the time of the MRI was 4.8 ± 3.2 (range 0 to 12). On the PedANAM, mean PCA was -2.3 ± 3.8 (range -11.7 to 1.4), and mean Multiscore was 7.3 ± 5.3 (range 1.6 to 21.4). One patient lacked SLEDAI data and another lacked PedANAM indices, resulting in 11 available for correlative analyses.
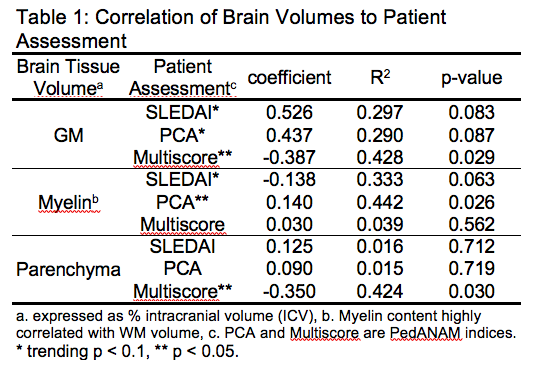
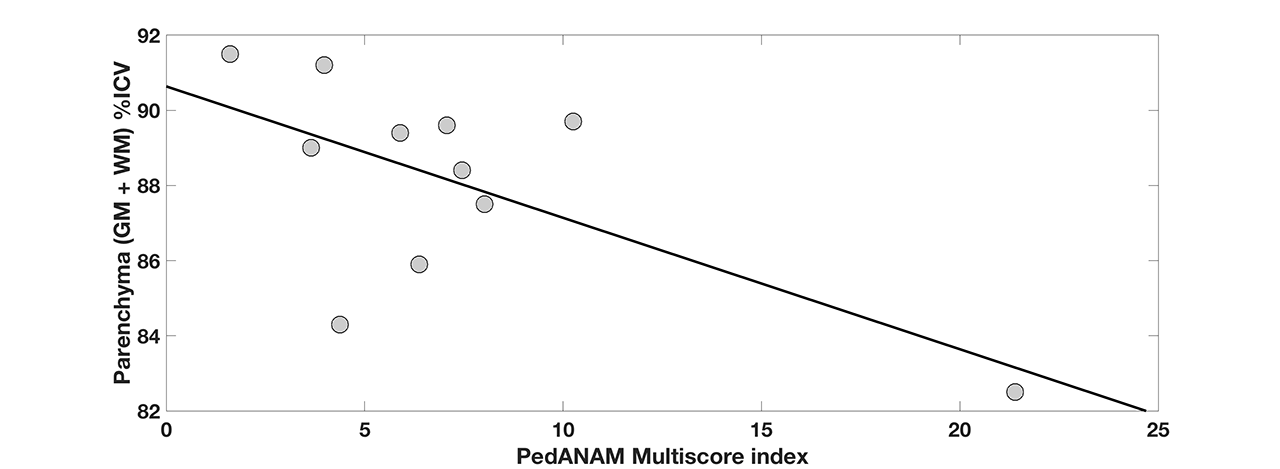
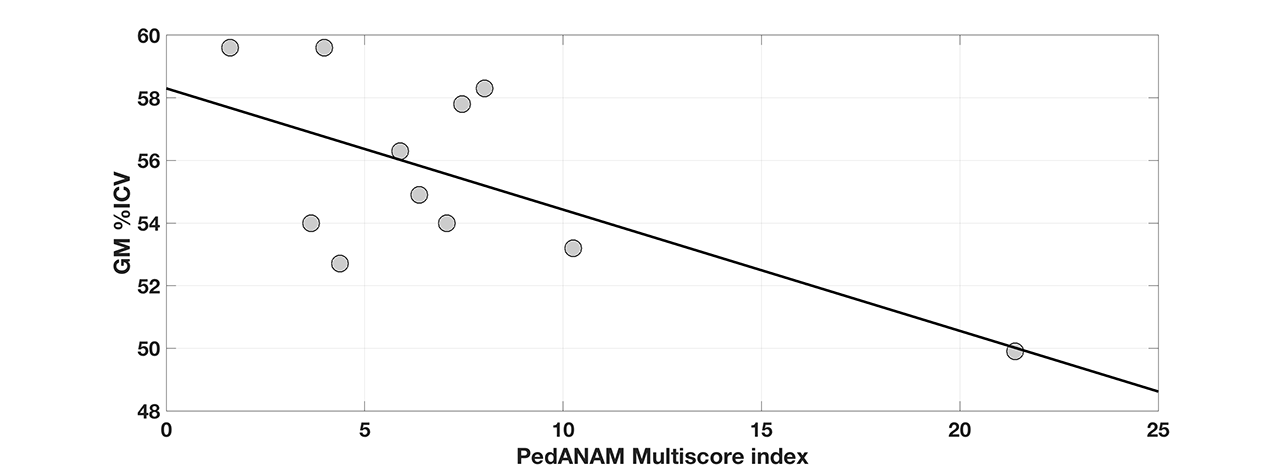
Regression results are summarized in Table 1. Total parenchymal volume as %ICV was found to significantly decrease as the Multiscore index increased (Figure 1). This relationship was driven by decreases in GM (Figure 2) rather than myelin (WM). Lack of correlation between parenchymal volume and PCA or SLEDAI could be at least partly explained by counterbalanced dependencies on GM and myelin volumes. WM and myelin volumes were highly correlated (R2=0.79) and gave similar outcomes. Age, gender, and race covariates were tested individually and found to not contribute significantly.
Conclusion: We present the results of whole-brain volumetric analysis in an initial group of cSLE patients referred for clinical brain MRI showing a significant association between neurocognitive measures and brain tissue class volumes. These outcomes motivate continued collection of clinical MRI data using our specialized protocol extensions with the aim of developing specific neuroimaging signatures for SLE for application to patient-centered care.
To cite this abstract in AMA style:
Brunner H, Mathur A, O'Brien W, DiFrancesco M. Tracking Whole-Brain Volumetric Trends in Childhood-onset Systemic Lupus Erythematosus Patients in the Clinical Setting by Magnetic Resonance Imaging [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/tracking-whole-brain-volumetric-trends-in-childhood-onset-systemic-lupus-erythematosus-patients-in-the-clinical-setting-by-magnetic-resonance-imaging/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tracking-whole-brain-volumetric-trends-in-childhood-onset-systemic-lupus-erythematosus-patients-in-the-clinical-setting-by-magnetic-resonance-imaging/