Session Information
Date: Tuesday, October 28, 2025
Title: (2437–2469) Systemic Lupus Erythematosus – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Photosensitivity lowers quality of life in patients with cutaneous lupus erythematosus (CLE) and puts patients with systemic lupus erythematosus (SLE) at risk of systemic disease flare. Janus kinase (JAK) inhibitors can reduce Type I interferons (IFNs) in the skin, where they are important drivers of photosensitivity. In addition, JAK inhibitors can interrupt neutrophil NETosis, a potentially important cell population in CLE. We thus examined the impact of JAK blockade in patients with a history of CLE.
Methods: We conducted a proof-of-concept mechanistic study in patients with a history of CLE, either in isolation or with associated SLE. Participants underwent phototesting with 0, 10, 20, 30, 40, 50, 60, 70 and 80 mJ/cm2 UVB prior to initiation of a 3-week course of 11 mg XR tofacitinib PO daily followed by repeat phototesting after drug completion. Biopsies were taken from unexposed skin, the initial minimal erythema dose (MED) site and from the site corresponding to the next highest UVB dose (MED+1) from initial and follow-up phototesting for mechanistic studies. The primary endpoint was the change in percentage of UVB-induced apoptotic epidermal cells from Day 1 (pre-treatment) to Day 26 (post-treatment). Safety and disease activity metrics were assessed.
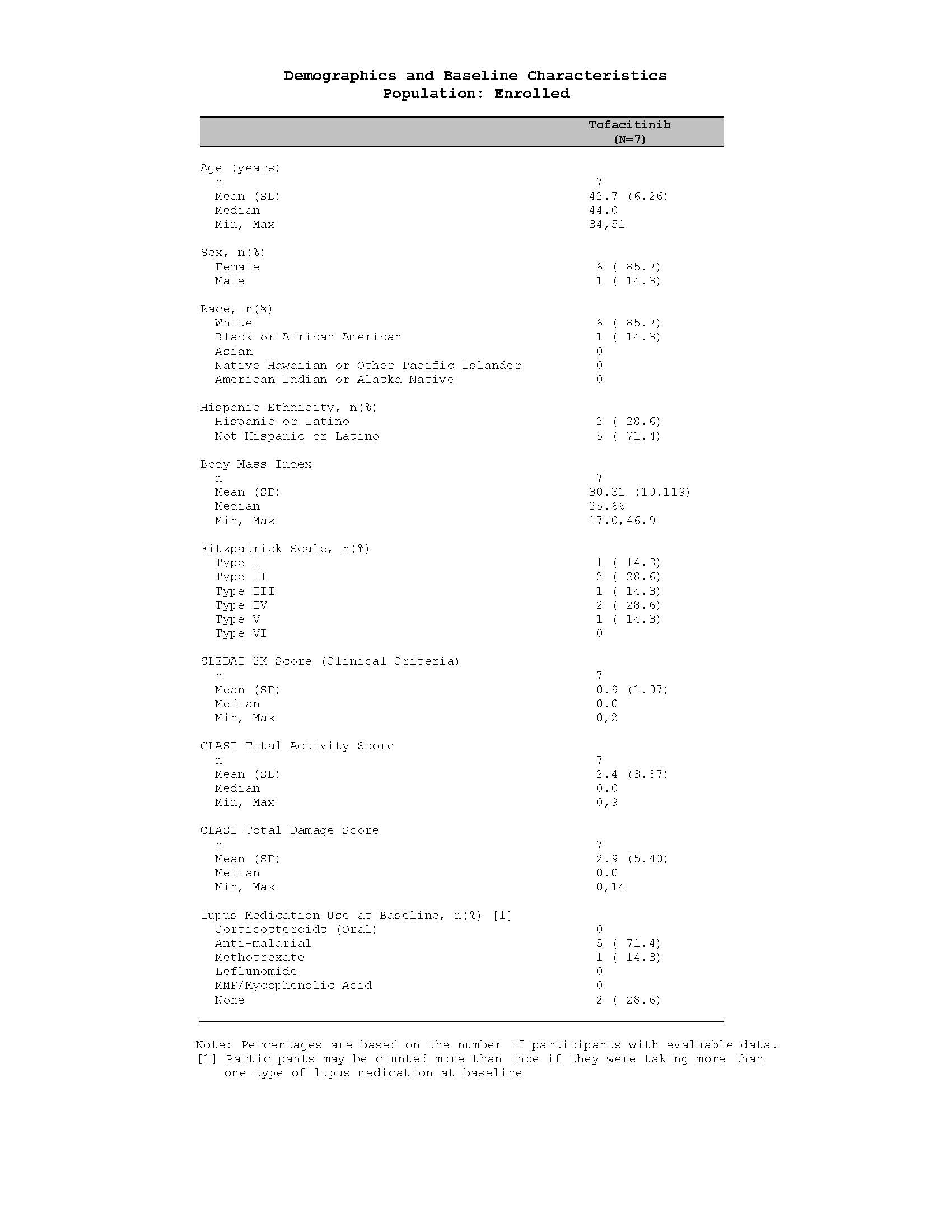
Results: Seven patients were enrolled and 6 patients completed the study. Participant data can be seen in Table 1. A single grade 2, unrelated adverse event (AE) was reported and no participant withdrew due to an AE. The mean change in percent of apoptotic epidermal cells following tofacitinib treatment was -17.03% (SD 8.355). Analyses of secondary outcomes comparing pre vs. post tofacitinib showed no change in MED, no change in CLASI activity and damage scores, and no change in SLEDAI. A varied response to tofacitinib was observed within and across participants in gene transcripts via bulk RNA sequencing for UVB-mediated cutaneous gene expression for IL6, IFNB, IFI44, TNFA, IL1B, and CXCL9. However, single cell spatial transcriptomics revealed that following tofacitinib treatment, there was a significant decrease (FDR 1.0E-03) in UVB-induced type I IFN-regulated genes in many cell populations, including keratinocytes and fibroblasts, and a reduction in genes regulating antigen presentation and cytotoxic T cell activation in myeloid cells, such as SIGLEC1, CCL5, CD1C, CD207, MX1, and IFI44L. All patients demonstrated a significant reduction from baseline in PMA-stimulated production of neutrophil extracellular traps (NETs) from circulating neutrophils following administration of tofacitinib, and there was a trend towards decreased neutrophil staining in the UVB-treated skin as well.
Conclusion: A 3-week course of tofacitinib was well-tolerated and reduced epithelial apoptosis after UVB exposure in patients with a history of CLE. Single cell resolution spatial transcriptomics identified cell-specific inflammatory gene reductions in the presence of tofacitinib following UVB exposure. The principal limitation of the trial was the small sample size. Additional studies are needed to investigate whether JAK inhibition is a viable strategy for reduction of photosensitivity and prevention of UVB-mediated skin and systemic disease flares.
To cite this abstract in AMA style:
Hurst A, Gharaee-Kermani M, Cai Y, Bogle R, Zhang L, Young A, Dobry C, Yalavarthi S, Knight J, Gudjonsson J, Tsoi A, Rohan P, Kibiy A, Boyle K, Byron M, Baird L, Kahlenberg J. Tofacitinib Lowers Markers of Photosensitivity in Patients with Cutaneous Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/tofacitinib-lowers-markers-of-photosensitivity-in-patients-with-cutaneous-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tofacitinib-lowers-markers-of-photosensitivity-in-patients-with-cutaneous-lupus-erythematosus/