Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Non-infectious uveitides (NIUs) include a heterogeneous group of sight-threatening and incapacitating conditions. Their correct management sometimes requires the use of immunosuppressive drugs (ISDs), prescribed in monotherapy or in combination. Several observational studies showed that the use of ISDs in combination could be more effective than their use in monotherapy. However, a direct comparison between these two treatment strategies has not been carried out yet.Objective:To analyze the effect of ISDs combination therapy (CT) on the response rate in patients with NIUs.
Methods: Patients attending a Uveitis Outpatient Clinic from a tertiary care center in Madrid, Spain, and prescribed with ISDs from 1991 to 2018 were included. Patients were assigned as controls or cases based on whether they were prescribed with ISDs in monotherapy (MT) or CT. ISD treatment changes during the observation period were also considered. The primary outcome was good therapeutic response (GTR), defined as the complete resolution of the eye inflammatory manifestations and oral corticosteroid dosage ≤10 mg of prednisone equivalent a day. Furthermore, this situation had to be maintained in at least two consecutive visits spanned at least 28 days. Several propensity score based and non-based weighting techniques for data balancing, followed by Cox regressions, were performed to estimate the effect of CT on the response rate. Random forest (RF) models and clinical appraisal were used to select the variables to be balanced.
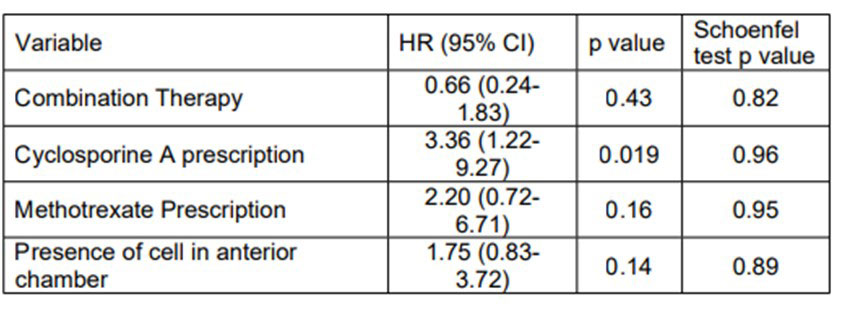
Results: 100 episodes of ISD prescription belonging to 73 patients were included in this analysis. In 32 episodes, patients were prescribed with CT (in 3 episodes CT was the initial therapeutic strategy; in 29, combination was the result to adding a second or third ISD). The most frequent drug used in MT was cyclosporine A (CYA; n=39), and the most frequent CT was synthetic + biological ISD (n=21). After RF, the number of previously used ISDs, the prescription of CYA, the dosage of oral corticosteroids at prescription, a previous ISD withdrawal due to inefficacy, and duration of disease were selected for balancing. In addition, after clinical appraisal, uveitis diagnosis, prescription with azathioprine, prescription with methotrexate, and eye activity features at prescription (presence of cells in anterior chamber, vitreous haze, macular edema, active chorioretinal lesions) were also balanced. The Energy balancing method showed the best balance for GTR. After Cox-regression, CT prescription did not show a statistically significant effect in the hazard of response (p=0.43; Table 1).
Conclusion: The use of CT in our study was not associated with a better therapeutic response in NIU patients compared with the prescription of MT. Considering that most CT episodes were the result of the addition of a new ISD in a patient already treated and still active, the effectiveness of CT as the initial therapeutic strategy remains unanswered.
To cite this abstract in AMA style:
Álvarez Hernández M, Madrid-García A, Gómez Gómez A, Borrego Sanz L, Méndez Fernández R, Arriola Villalobos P, Pato Cour E, Díaz Valle D, Rodriguez-Rodriguez L. To Combine or Not to Combine: Influence of Immunosuppressive Drug Combination in the Induction of Therapeutic Response in Non-infectious Uveitis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/to-combine-or-not-to-combine-influence-of-immunosuppressive-drug-combination-in-the-induction-of-therapeutic-response-in-non-infectious-uveitis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/to-combine-or-not-to-combine-influence-of-immunosuppressive-drug-combination-in-the-induction-of-therapeutic-response-in-non-infectious-uveitis/