Session Information
Date: Sunday, November 10, 2019
Title: 3S112: Vasculitis – Non-ANCA-Associated & Related Disorders I: Miscellaneous Disorders (945–950)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Deficiency of adenosine deaminase 2 (DADA2) is an autosomal recessive disease caused by biallelic loss-of-function mutations in the ADA2 gene . Over 60 pathogenic mutations have been identified in all domains of the resultant protein, adenosine deaminase 2 (ADA2). ADA2 is an endothelial cell growth factor and promotes M2 macrophage differentiation, leading to a chronic inflammatory state. Known manifestations of ADA2 deficiency include recurrent fevers, immunodeficiency, livedo racemosa, polyarteritis nodosa, and early-onset stroke – many of which may worsen with acute or recurrent disease flares. An earlier study by our group demonstrated a reduced risk of recurrent strokes in 15 patients with DADA2 secondary to anti-tumor necrosis factor (TNF) treatment. The purpose of this abstract is to provide additional stroke data before and after initiation of anti-TNF treatment on a larger cohort since the initial publication.
Methods: A single center study evaluated 49 patients with molecularly diagnosed pathogenic mutations in ADA2. Medical records were manually reviewed. Stroke incidences were only included if reported as confirmed by imaging. Patients were subdivided by past incidence of stroke and initiation of anti-TNF treatment such as etanercept, adalimumab, golimumab, or infliximab. Cumulative duration of the disease was calculated for each patient before and after initiation of anti-TNF treatment, i.e. time since birth and time to present record, respectively.
Results: Of the 49 patient cohort, 24 had documented histories of strokes, all of which are currently on anti-TNF treatment. The median age of first stroke was 5.0 years (range, 0.48 to 21) with a median of 2 strokes per patient (range, 1 to 10). Before initialization of anti-TNF treatment, the patients had a cumulative disease duration of 8,997 patient months and a cumulative total of 69 strokes. After the initiation of anti-TNF treatment there have been no reported strokes over a period of 2,024 patient-months with a median duration of 56 months (range, 1.7 to 153) (p < 0.001).
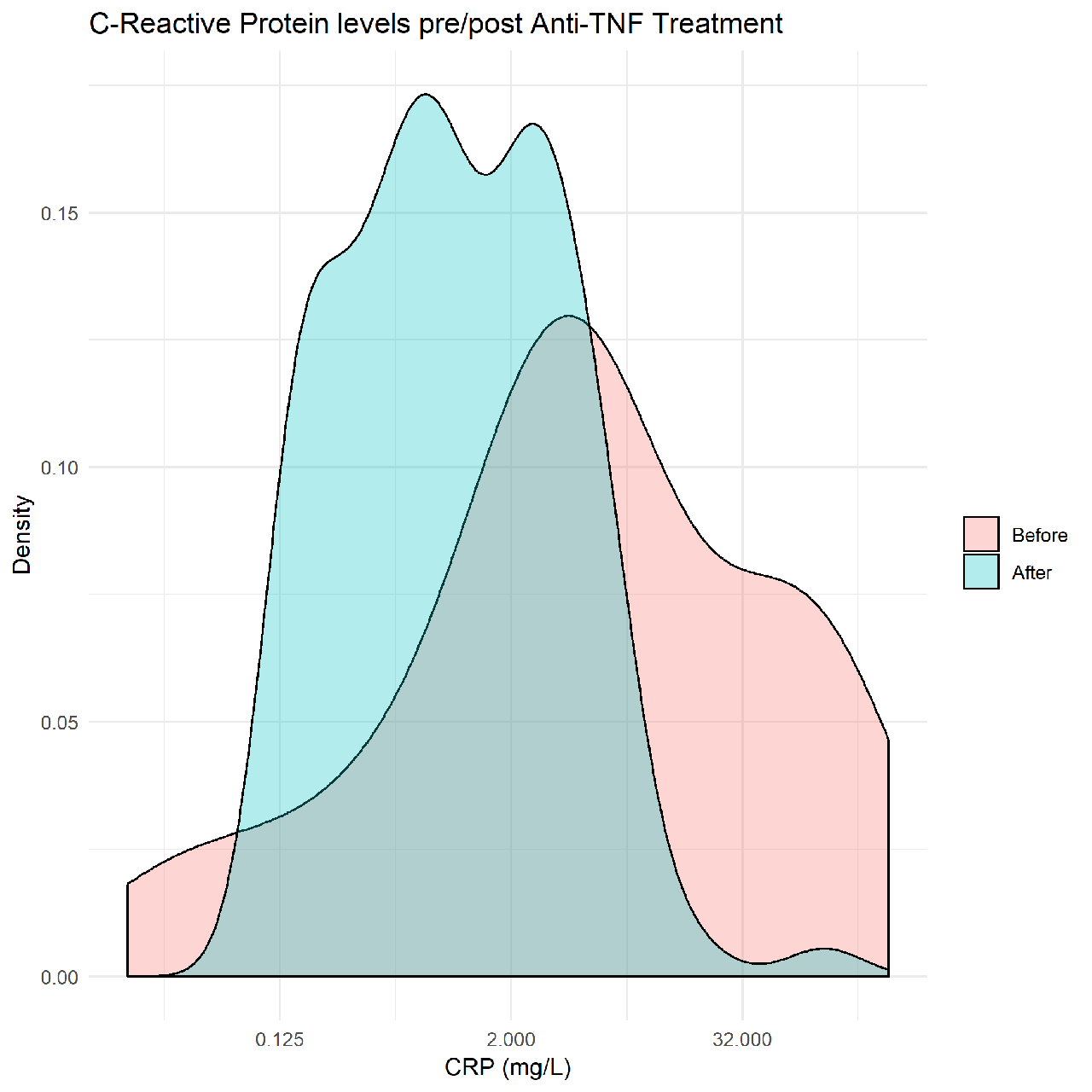
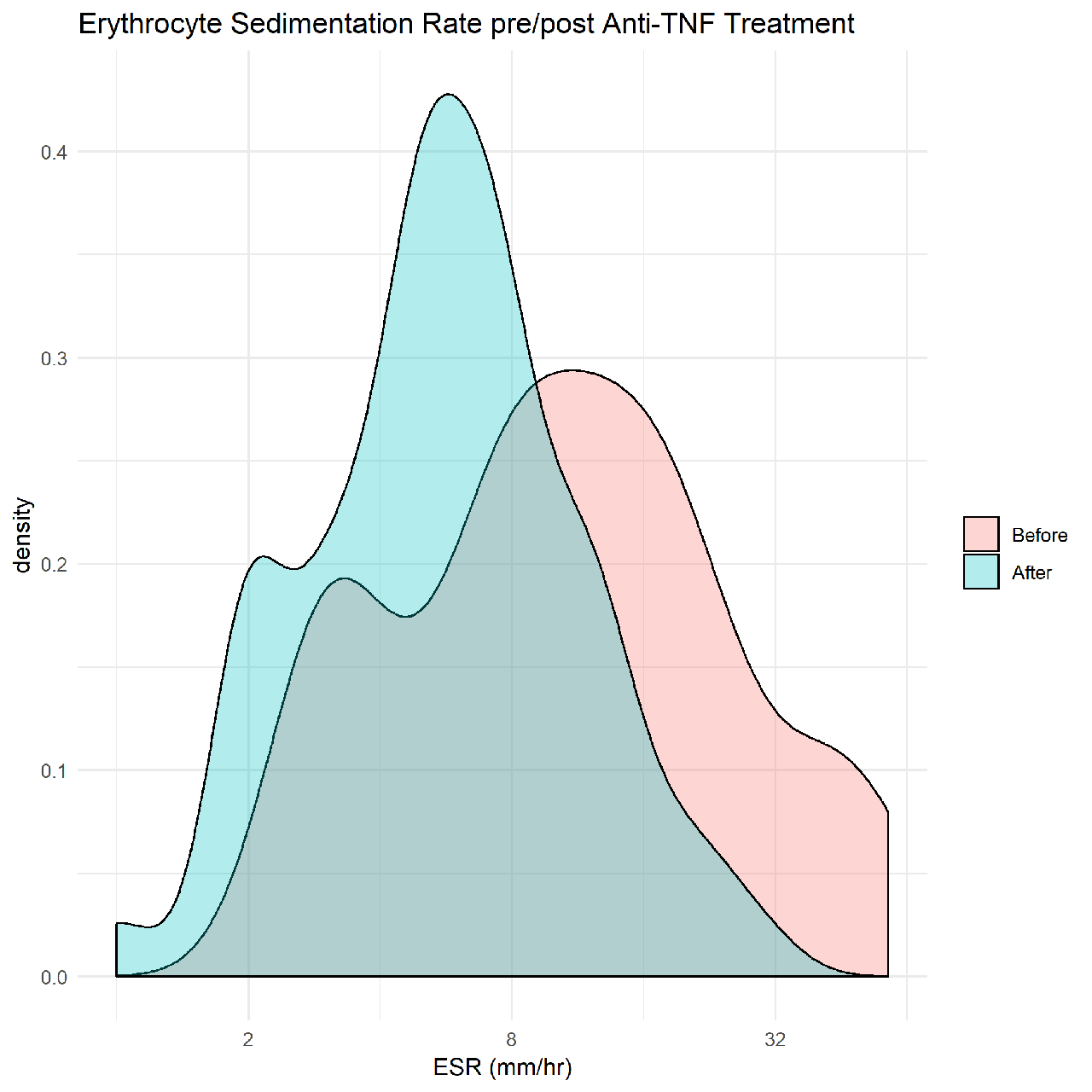
Conclusion: Patients with DADA2 have a high risk for early-onset strokes. In a cohort of 49 patients with DADA2, 24 patients with history of stroke have all began anti-TNF treatment. Thus far these patients have experienced no recurrent strokes over a cumulative period of 2,024 patient months. This suggests anti-TNF treatment plays a key role in the reduction of strokes in patients with DADA2. Aside from stroke reduction, we have seen a normalization in key lab values such as CRP (Figure 1), ESR (Figure 2), Hgb and HCT which indicates an overall decrease in inflammation. Other lab indicators such as neutropenia and red cell aplasia remain variable or unchanged, suggesting additional targeted therapy may further benefit DADA2 patients.
To cite this abstract in AMA style:
Laird R, Hoffmann P, Barron K, Stone D, Nehrebecky M, Jones A, Romeo T, Toro C, Soldatos A, Cudrici C, Kastner D, Ombrello A. TNF Inhibitor Treatment and Dramatic Stroke Risk Reduction in Patients with Deficiency of Adenosine Deaminase 2 [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/tnf-inhibitor-treatment-and-dramatic-stroke-risk-reduction-in-patients-with-deficiency-of-adenosine-deaminase-2/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tnf-inhibitor-treatment-and-dramatic-stroke-risk-reduction-in-patients-with-deficiency-of-adenosine-deaminase-2/