Session Information
Date: Monday, November 18, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Pathogenic inflammation in psoriatic arthritis (PsA) includes TNF pathway engagement, and this is associated with morbidity. Recently, we observed lower absolute lymphocyte count (ALC) is associated with greater mortality in the setting of Rheumatoid Arthritis, and that TNF-inhibitor (TNFi) therapy results in an increase in ALC in patients treated with methotrexate. ALC is a commonly obtained immune marker that may lend insight into the immunopathogenesis of PsA. The effect of TNFi on ALC and the relationship between ALC and mortality in patients with PsA is not known. Here we evaluated the effect of TNFi therapy on ALC and subsequent mortality in patients with PsA.
Methods: Using the VA Corporate Data Warehouse, we identified patients with PsA started on TNFi therapy between 2010 and 2015, who remained on treatment at least 90 days, and who had outpatient CBC labs both in the year before and 3-24 months after therapy initiation. We identified a total of 1923 patients who were seen in Rheumatology Clinics, and matched these by age, sex, race and ethnicity with controls (without TNF-inhibitor, with repeated CBC labs in the same time window, and without medication changes between labs). To evaluate potential connections between ALC and immunopathogenesis, in local cohorts of patients with PSA (n=27) and controls (n=22) we measured serum/plasma levels of IL6, sTNFR2, TNF, CRP, and oxidized LDL (total oxLDL, and MDA, CML and HNE subtypes) by ELISA.
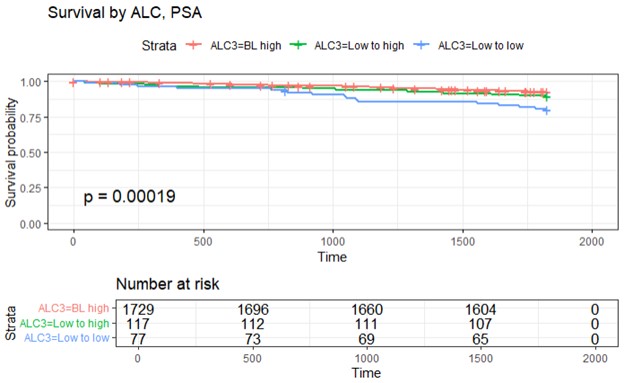
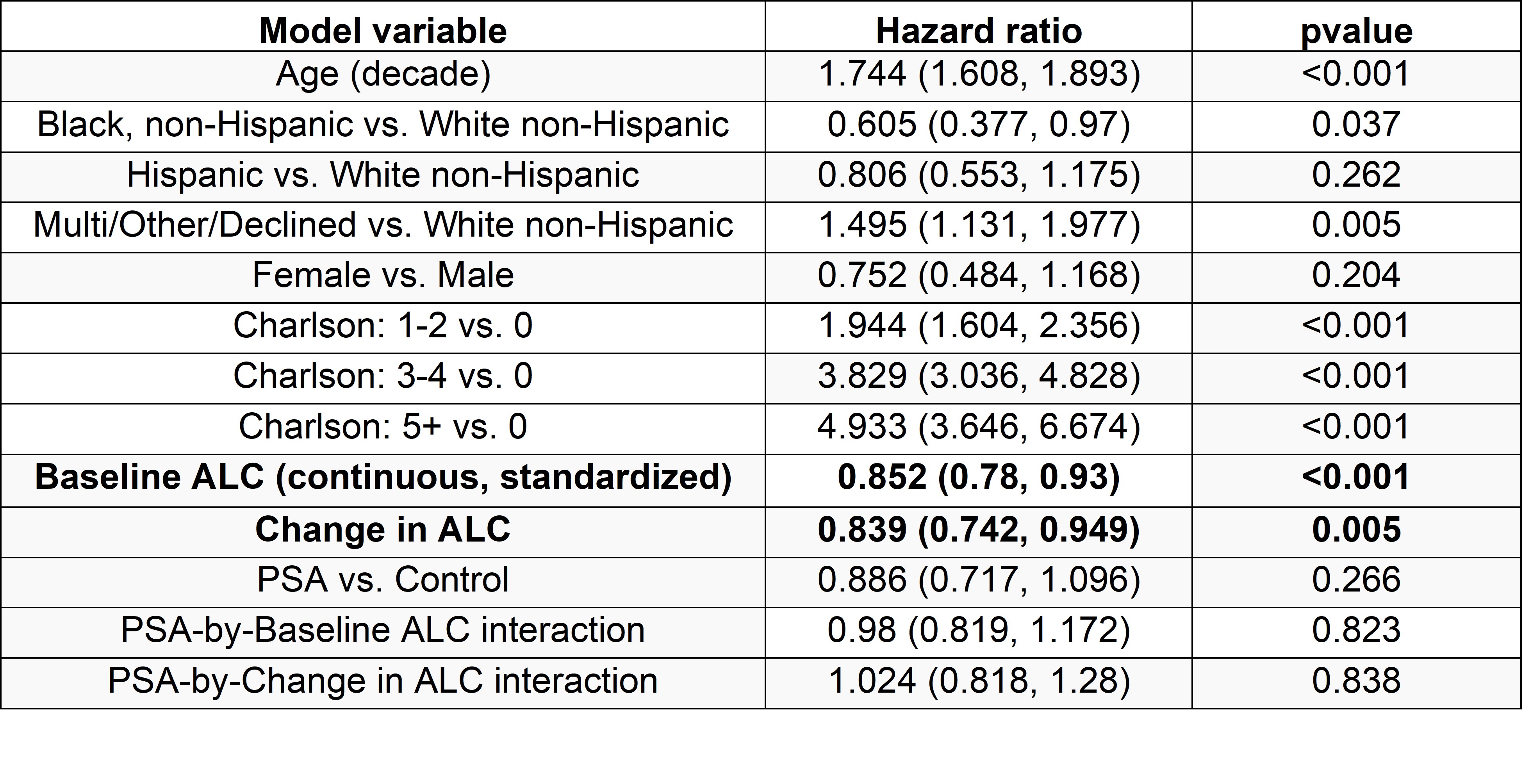
Results: Among 1923 patients with PsA, ALC increased by a mean of 0.22×103 cell/ul (95% CI = 0.19, 0.25) following TNF initiation, while in controls there was minimal change in ALC over the same time period (0.01×103 cell/ul, 95% CI = 0.00, 0.02). Survival curves differed significantly among PsA subjects with a baseline ALC above 1.2×103 cell/ul, a baseline below 1.2×103 cell/ul that remained low after start of TNFi, and a baseline below 1.2×103 cell/ul that increased to above 1.2×103 cell/ul on therapy (p=0.0002, Figure 1). In a Cox proportional hazards model that included PsA and matched control subjects, higher ALC at baseline and increased ALC at follow-up were significantly associated with higher subsequent survival. Interaction effects of ALC with PSA were not detected, suggesting similar mortality benefits of higher ALC in both PSA and control subjects where ALC increased on average in PSA subjects and remained stable in controls (Table 1).
In our local PsA and control cohorts where immune sampling was performed we observed higher sTNFR2 plasma levels in PsA compared to control groups (p=0.002), and in those with PsA sTNFR2 levels correlated with TNF levels (r= 0.46, p=0.048, n=19). Comparing those in the PsA group on vs. not on TNFi therapy, those on TNFi had lower plasma levels of IL6 (p=0.03). At the same time oxLDL levels positively correlated with ESR and CRP levels and negatively correlated with ALC in those with PsA not on TNFi.
Conclusion: TNFi therapy increases the peripheral blood ALC in patients with psoriatic arthritis, and this is associated with lower subsequent mortality. Mechanisms underlying this relationship are unknown, though further investigation of the effects of TNFi on oxLDL, ESR, CRP and ALC are warranted.
To cite this abstract in AMA style:
Kostadinova L, Wilson B, Siddiqui H, Behrens S, Gupta A, O'Mara M, Nahra V, Makandura M, Malakooti S, Mattar M, Zidar D, Anthony D. TNF Inhibitor Therapy Increases Absolute Lymphocyte Count Which Is Associated with Lower Mortality in Patients with Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/tnf-inhibitor-therapy-increases-absolute-lymphocyte-count-which-is-associated-with-lower-mortality-in-patients-with-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tnf-inhibitor-therapy-increases-absolute-lymphocyte-count-which-is-associated-with-lower-mortality-in-patients-with-psoriatic-arthritis/