Session Information
Date: Monday, November 9, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Bench to Bedside
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Vitamin D is correctly classified as a sterol-hormone rather than a vitamin (Semin Nephrol 1986;6:4-20). It has multiple immunomodulatory effects, as well as cardiovascular and hematologic benefits (such as reduction in thrombosis). In SLE patients who are vitamin D insufficient/deficient, vitamin D supplementation clearly improves proteinuria (Arthritis Rheum 65:1865-71, 2013) with a plateau at a 25(OH)-vitamin D level of 40 ng/mL. In fact, vitamin D helps proteinuria in diverse renal diseases (Int J Environ Res Public Health 2018;15:1773).
Methods: The SLE patients met revised ACR or SLICC classification criteria. This analysis included 73,221 person months (6,102 person years) from 1,220 patients (93% female, 38% African-American, 52% Caucasian). 48.5% were diagnosed at age < 30 years. Vitamin D levels were measured regularly starting mid-2009. Renal insufficiency was defined as creatinine (CR) ≥1.5 mg/dl or < 50% function. For this analysis, a dataset with one record for each month of follow up for each person was constructed. Mean prior vitamin D levels were calculated over all previous months. Patients were followed from the first measure of 25(OH)-vitamin D level to first incident of renal insufficiency or their last recorded visit. To calculate the rate of renal insufficiency in each demographic or clinical subgroup, the number of renal insufficiency events was divided by the number of person months at risk and then converted to rates per 1,000 person years. Pooled logistic regression was used to assess the relationship between vitamin D blood levels and rates of renal insufficiency.
Results: Table 1 shows the association between patient characteristics and the rate of renal insufficiency. Renal insufficiency was more common in males, African-Americans and obese patients. Table 2 shows the association between Vitamin D level tertiles and the rate of renal insufficiency. There was a significantly elevated risk of renal insufficiency among those in the extremely low levels of 25(OH)-vitamin D (< 20 ng/mL). Figure 1 shows the trend of rates of renal insufficiency by vitamin D levels. The effect of 25(OH)-vitamin D < 20 ng/mL was clearly shown regardless if we used first, most recent or mean level of 25(OH)-vitamin D. Results were adjusted for race, age, sex and BMI.
Conclusion: The benefit of vitamin D supplementation to reduce proteinuria in SLE brought the benefit of this sterol-hormone as an immunomodulatory to the forefront. Now our data show that very low 25(OH)-vitamin D levels < 20 ng/mL are associated with renal insufficiency (adjusted for ethnicity, as African-Americans have lower levels).
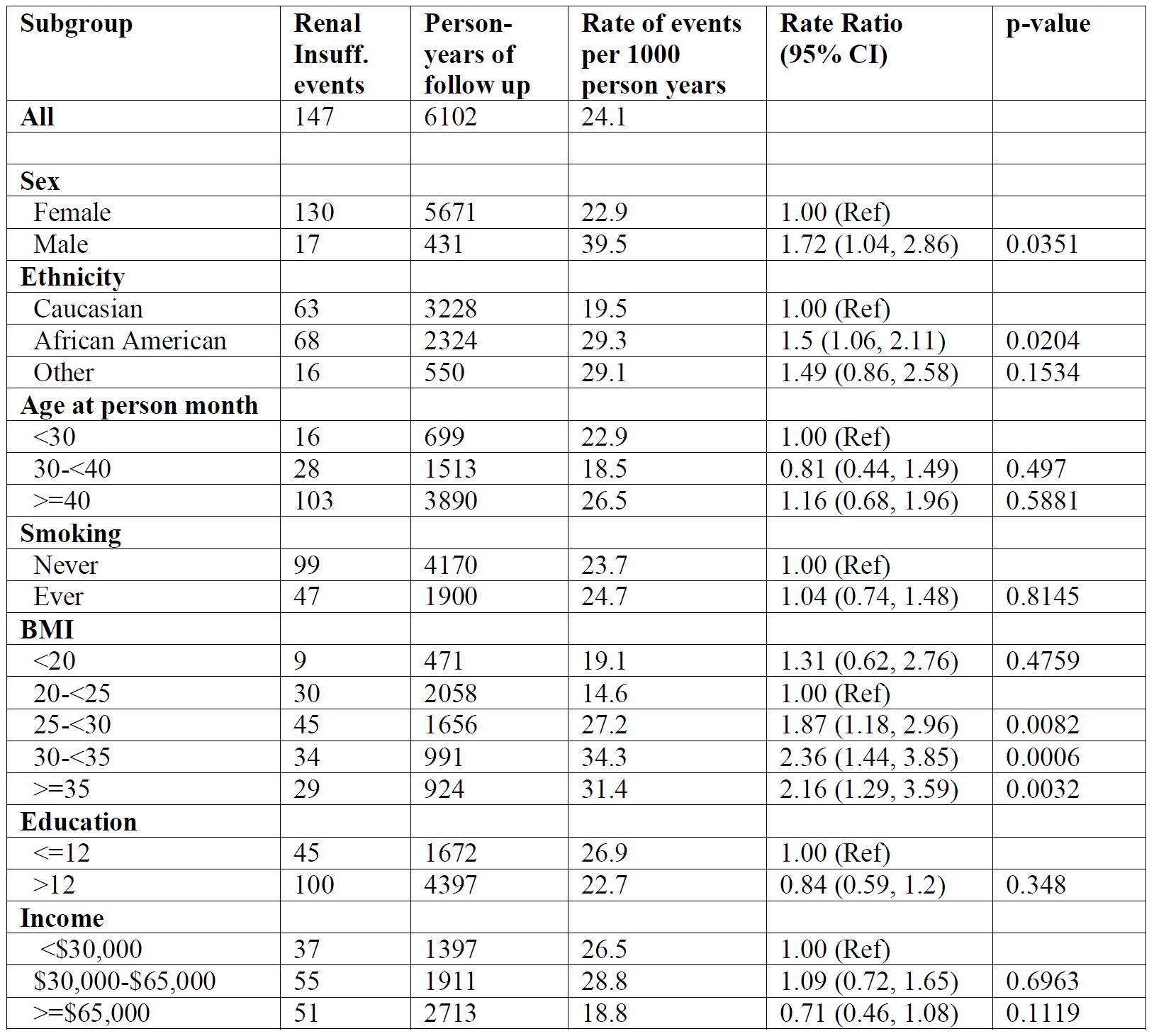 Table 1: Rates of renal insufficiency events by demographics and patients characteristics
Table 1: Rates of renal insufficiency events by demographics and patients characteristics
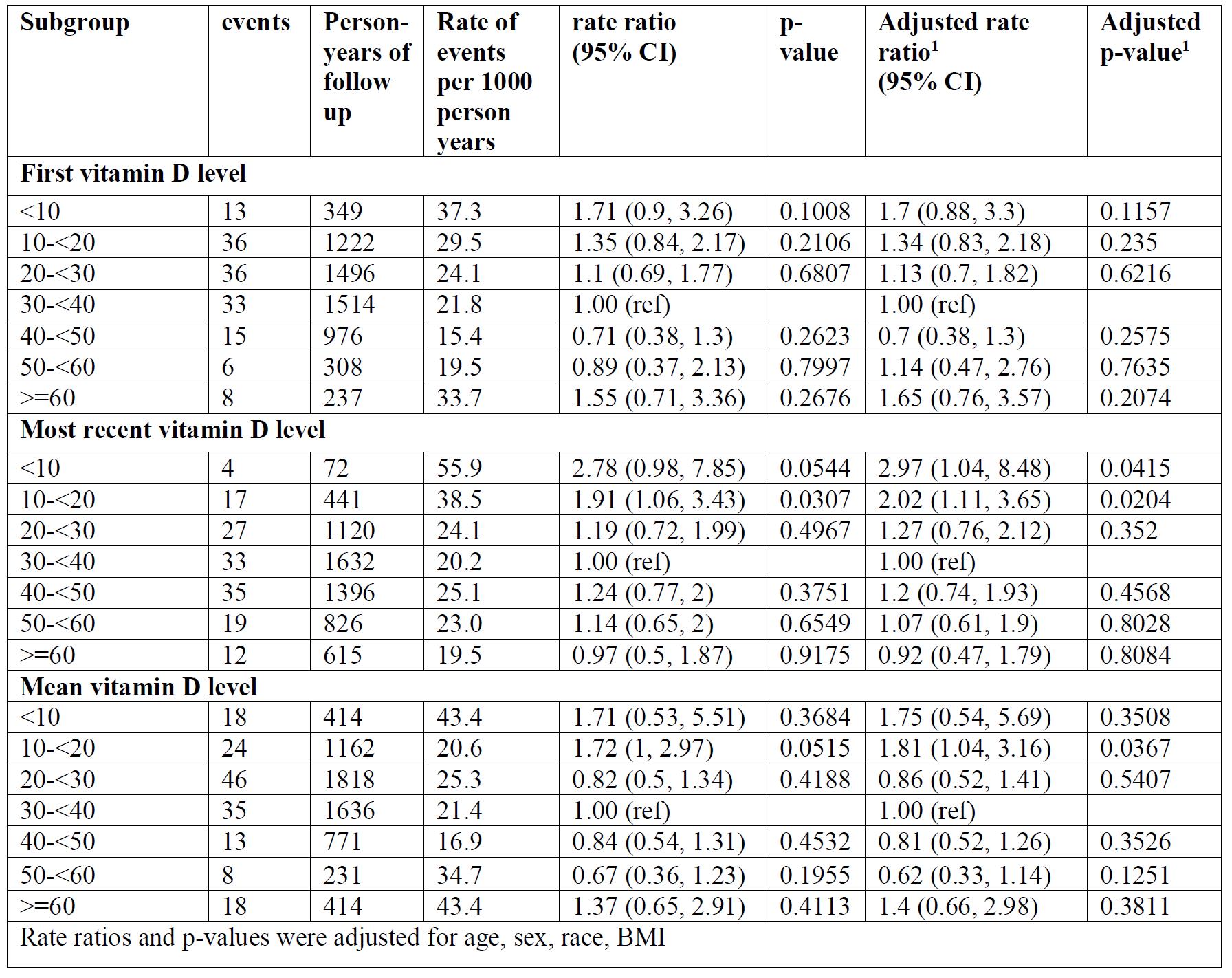 Table 2: Rates of renal insufficiency events by 25(OH)-vitamin D levels
Table 2: Rates of renal insufficiency events by 25(OH)-vitamin D levels
 Figure 1: Rates of renal insufficiency by 25(OH)-vitamin D levels
Figure 1: Rates of renal insufficiency by 25(OH)-vitamin D levels
To cite this abstract in AMA style:
Petri M, Li J, Goldman D. Time to Renal Insufficiency Based on 25(OH)-Vitamin D Levels [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/time-to-renal-insufficiency-based-on-25oh-vitamin-d-levels/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/time-to-renal-insufficiency-based-on-25oh-vitamin-d-levels/
