Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: This study aimed to evaluate the clinical characteristics of thrombocytosis, its relationship with disease activity and joint involvement, and its influence on the effectiveness of biologic and targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) in patients with rheumatoid arthritis (RA).
Methods: Data from 2,104 patients with RA from the Korean College of Rheumatology Biologics and Targeted Therapy registry were analyzed. Thrombocytosis was defined as a platelet count >450 × 10⁹/L. Baseline demographics, comorbidities, laboratory results, joint involvement, and disease activity indices (DAS28, SDAI, CDAI, RAPID3, ESR, CRP) were compared between patients with and without thrombocytosis. Responses to b/tsDMARDs over 1 year were assessed using ACR and EULAR criteria. Logistic regression identified independent predictors of thrombocytosis.
Results: Thrombocytosis was found in 97 patients (4.6%). Compared to those with normal platelet counts, these patients had significantly higher ESR, CRP, and WBC counts, lower hemoglobin, higher disease activity scores, and more frequent large joint involvement. Anemia, diabetes, obesity, and bronchiolitis obliterans organizing pneumonia were also more common. At 1 year, ACR70 response rate was significantly higher in the thrombocytosis group (39.2% vs. 29.0%, p=0.041), while ACR20 and ACR50 responses were similar. IL-6 inhibitors, particularly tocilizumab, were more effective in patients with thrombocytosis, achieving higher ACR20/50/70 responses and greater reductions in platelet count and inflammatory markers. Other b/tsDMARDs, such as TNF and JAK inhibitors displayed favorable but non-significant trends. Multivariate logistic regression identified higher WBC count, lower hemoglobin, and elevated ESR as independent predictors of thrombocytosis in RA.
Conclusion: Thrombocytosis in RA indicates increased disease activity and greater joint involvement. Monitoring platelet counts helps assess disease severity and tailor treatments, particularly IL-6 targeting therapies.
 Table. Risk factors for thrombocytosis in patients with RA were analyzed using logistic regression analysis.
Table. Risk factors for thrombocytosis in patients with RA were analyzed using logistic regression analysis.
SJC, swollen joint count; TJC, tender joint count; WBC, white blood cell; ESR, erythrocyte sediment rat; CRP, C-reactive protein; DAS28-CRP, Disease Activity Score in 28 joints based on C-reactive protein; SDAI, Simple Disease Activity Index; RAPID, Routine Assessment of Patient Index Data; DM, diabetes mellitus; BOOP, bronchiolitis obliterans organizing pneumonia; PGA, patient’s global assessment; PhGA, physician’s global assessment.
*statistically significant (p < 0.005).
** statistically significant (p < 0.010).
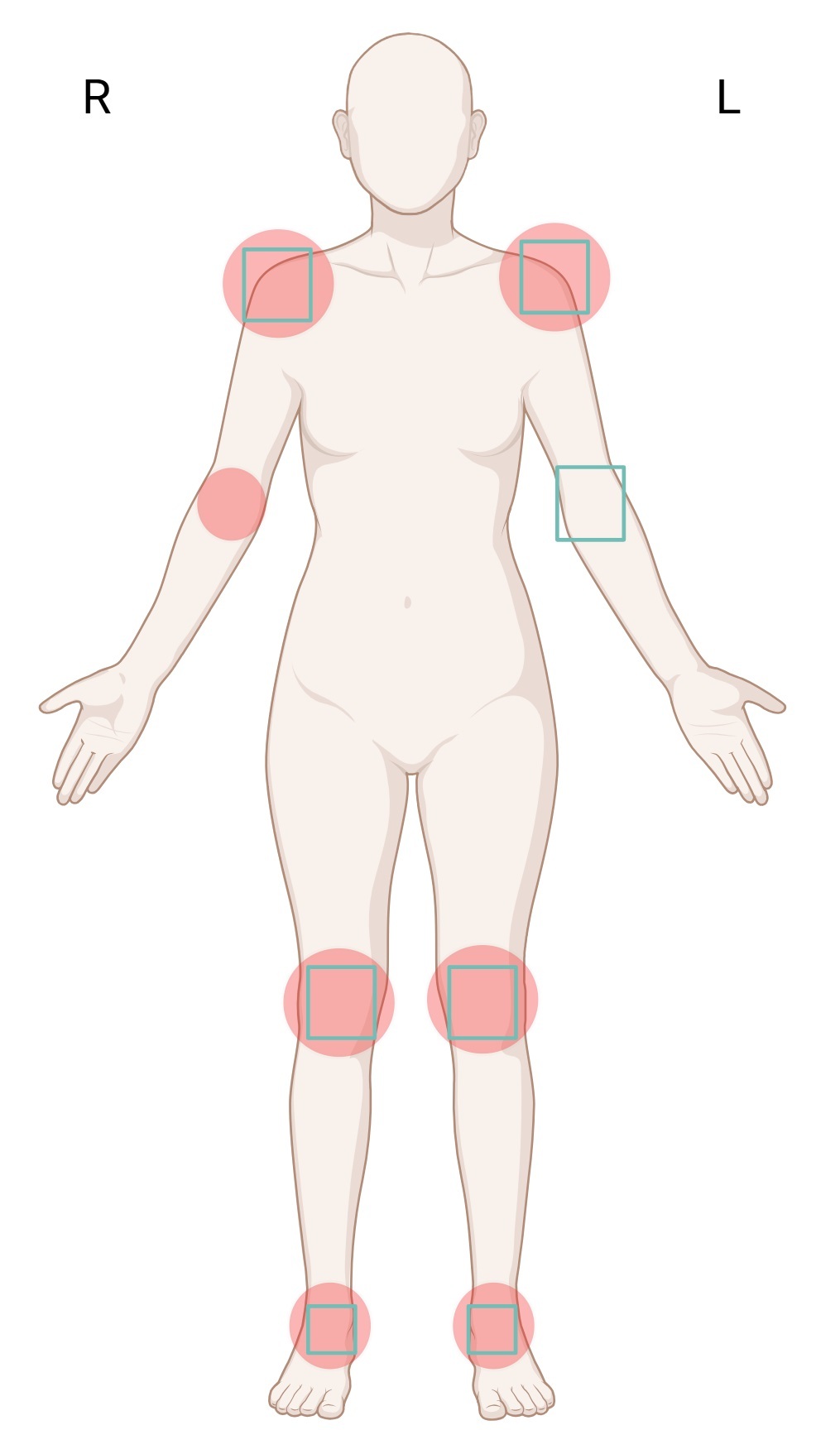 Figure. Involvement of swollen and tender joints in the thrombocytosis group.
Figure. Involvement of swollen and tender joints in the thrombocytosis group.
Swollen and tender joint involvement was more frequent in the thrombocytosis group. Transparent red circles indicate greater involvement of swollen joints, while green squares represent joints with increased tenderness in the thrombocytosis group.
.jpg) Figure. ACR response according to b/tsDMARDs.
Figure. ACR response according to b/tsDMARDs.
ACR, American College of Rheumatology; b/tsDMARDs, biologic and targeted synthetic disease-modifying antirheumatic drugs; TNF, tumor necrosis factor; JAK, Janus kinase.
*statistically significant (p < 0.005).
To cite this abstract in AMA style:
Kim S, Lee k. Thrombocytosis Predicts Response to Biologic and Targeted Synthetic DMARDs in Rheumatoid Arthritis: Data from the Korean KOBIO Registry [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/thrombocytosis-predicts-response-to-biologic-and-targeted-synthetic-dmards-in-rheumatoid-arthritis-data-from-the-korean-kobio-registry/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/thrombocytosis-predicts-response-to-biologic-and-targeted-synthetic-dmards-in-rheumatoid-arthritis-data-from-the-korean-kobio-registry/
