Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Thrombocytopenia is one of the hematological abnormalities that can occur in patients with systemic lupus erythematosus (SLE), and it has been shown to affect outcomes of SLE. The aim of this meta-analysis is to compare clinical characteristics of SLE patients with and without thrombocytopenia, and to assess the latter’s impact on prognosis.
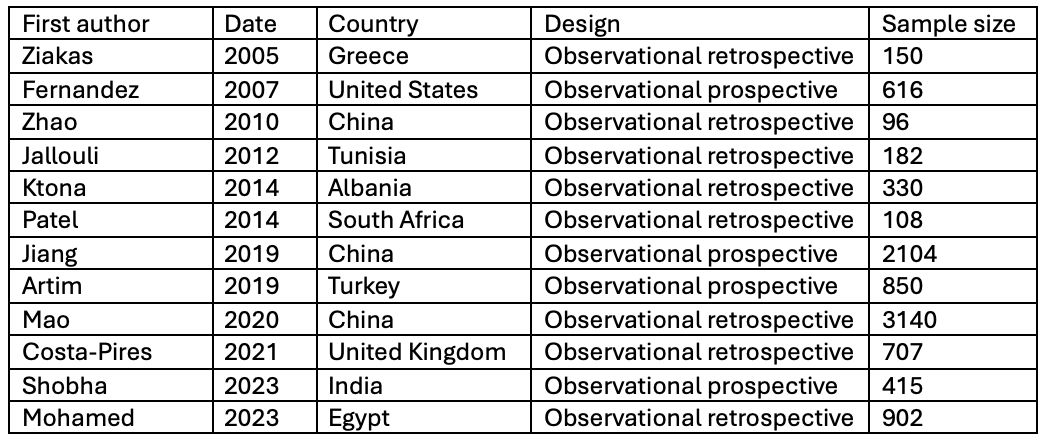
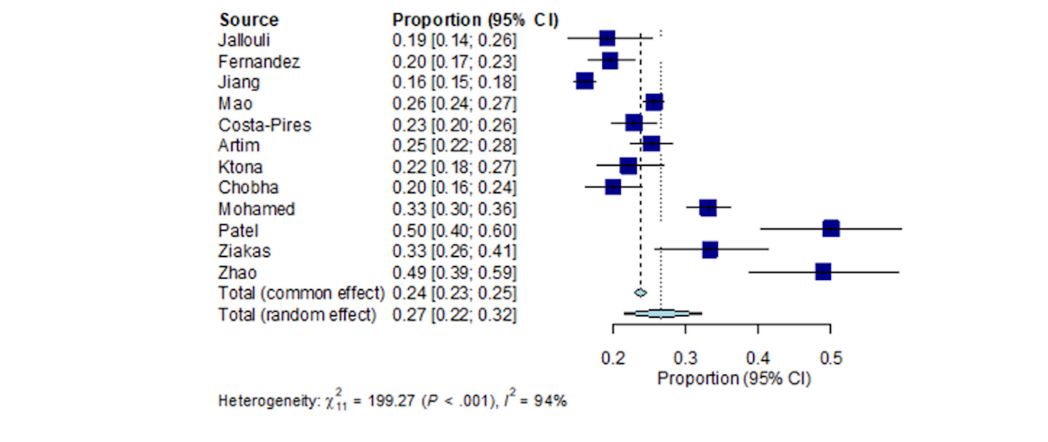
Methods: A literature search was conducted through the PUBMED database from inception to date to identify eligible studies comparing patients with SLE with and without thrombocytopenia. Studies were excluded if there was no comparison to control patients with no thrombocytopenia. In addition, we searched the reference lists of published articles and international conference abstracts manually to ensure a broad comprehensiveness of the bibliography. A forest plot was used to compare odds ratios (95% CI) of NPSLE manifestations by age group. Study heterogeneity was assessed using I2.
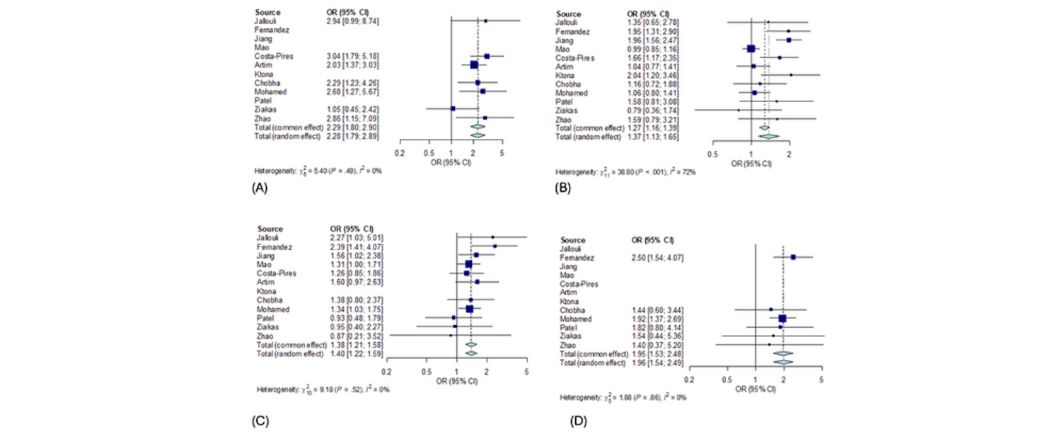
Results: Twelve observational studies were included comprising a total of 2285 SLE patients with thrombocytopenia and 7315 SLE patients without. The frequency of thrombocytopenia in SLE patients was 27% (OR: 0.27, 95%CI: 0.22-0.32, I2=94%) (Figure 1). Compared with SLE patients without thrombocytopenia, those with thrombocytopenia more commonly had associated autoimmune hemolytic anemia (AIHA) (OR: 2.28, 95%CI: 1.79-2.89, I2=0%) (Figure 2A), leukopenia (OR: 1.92, 95%CI: 1.68-2.19, I2=0%), lymphopenia (OR: 1.40, 95%CI: 1.07-1.83, I2=59%) and low C3 levels (OR: 1.71, 95%CI: 1.18-2.46, I2=53%). They also had higher rates of nephritis (OR: 1.37, 95%CI: 1.13-1.65, I2=72%) (Figure 2B), central nervous system (CNS) involvement (OR: 1.40, 95%CI: 1.22-1.59, I2=0%) (Figure 2C), and antiphospholipid syndrome (APS) (OR: 1.54, 95%CI: 1.28-1.85, I2=0%). On the other hand, photosensitivity was less frequent in patients with thrombocytopenia (OR: 0.83, 95%CI: 0.70-0.98, I2=14%). Other clinical and serological findings were similar in SLE patients with and without TP. Mortality data were eligible in 6 studies. Thrombocytopenia was also associated with higher mortality rates (OR: 1.96, 95%CI: 1.54-2.49, I2=0%) (Figure 2D).
Conclusion: In this study, we demonstrate convincing evidence for some differences between SLE patients with and without thrombocytopenia. Our study showed that in patients with SLE, thrombocytopenia was significantly associated with other hematological abnormalities, lower C3 levels, higher rates of kidney and CNS involvement, as well as APS. Our results also highlight that thrombocytopenia played an important prognostic factor in SLE patients, as its presence was associated with higher mortality.
To cite this abstract in AMA style:
Matar A, Pamuk O. Thrombocytopenia and Systemic Lupus Erythematosus: A Meta-analysis of Observational Studies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/thrombocytopenia-and-systemic-lupus-erythematosus-a-meta-analysis-of-observational-studies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/thrombocytopenia-and-systemic-lupus-erythematosus-a-meta-analysis-of-observational-studies/