Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: In rheumatoid arthritis (RA), initiation of treatment within the window of opportunity, i.e. 12 weeks after symptom onset, results in higher remission rates, and less radiographic progression and functional impairment. In contrast, in psoriatic arthritis (PsA) a diagnostic delay of 1-2 years is still common. PsA guidelines state that DMARDs should be started early, with a maximum delay of 1 year. However, it is unknown whether a shorter delay of 12 weeks yields better clinical outcomes. We aimed to investigate what the window of opportunity is in PsA.
Methods: All newly diagnosed, DMARD naïve PsA patients who participated in the Dutch southwest Early PsA cohort (DEPAR) were included (n=855). First, we calculated total delay, and then split this into patient and general practitioner (GP) delays to assess where potential gains could be made. Thereafter, patients were categorized in 3 groups, based upon total delay:
- < 12 weeks delay (early diagnosis)
- 12-52 weeks delay (late diagnosis)
- > 52 weeks delay
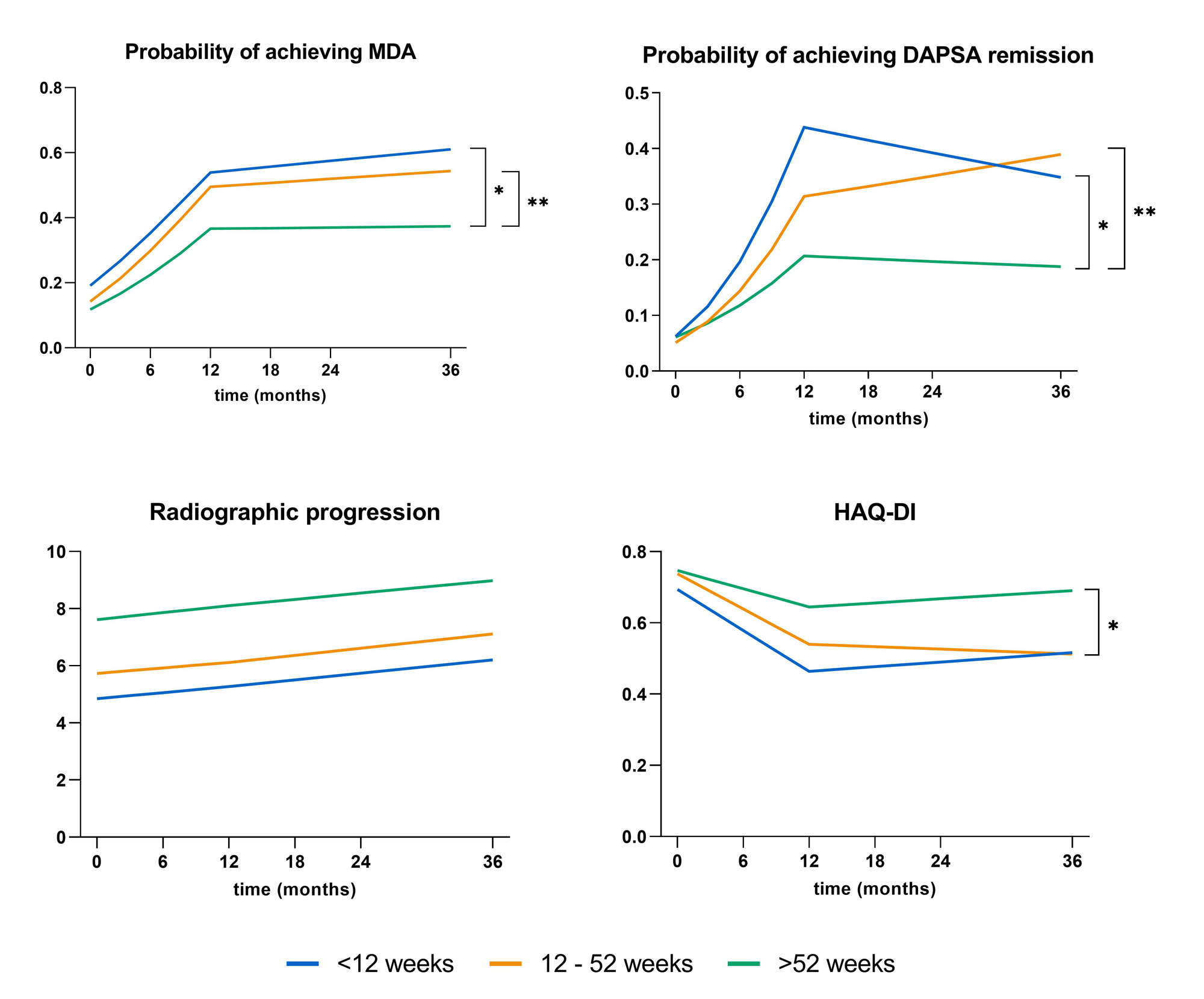
Aforementioned groups were compared on their probability of achieving Minimal Disease Activity (MDA) and Disease Activity in PSoriatic Arthritis (DAPSA) remission, defined as DAPSA < 5. We also assessed differences in radiographic progression and functional impairment. Radiographic progression is measured with the modified Sharp van der Heijde score (mTSS), while functional impairment is measured with the Health Assessment Questionnaire–Disability Index (HAQ-DI). Mixed models were used to compare outcomes over time (3 years).
Results: Median total delay was 42.0 weeks. Patient and GP delay were 4.4 and 18.0 weeks, respectively. PsA patients with > 52 weeks delay were more often female, had less swollen joints and lower CRP and ESR. They also more often had enthesitis. In contrast, no baseline differences were found between early and late diagnosis groups, respectively < 12 weeks and 12-52 weeks. The group with > 52 weeks delay was significantly less likely to achieve MDA and DAPSA remission over 3 years of follow-up compared to both the early and late diagnosis groups (Figure 1). The > 52 weeks delay group also scored significantly worse on HAQ-DI than the early diagnosis group. Radiographic progression did not differ significantly between groups. Although all outcomes were numerically better in PsA patients who were diagnosed within 12 weeks compared to those with a diagnosis within 52 weeks, no significant differences were found (Figure 1).
Conclusion: Early referral and diagnosis is associated with better clinical outcomes. Therefore, disease outcomes of PsA patients may improve with timely referral to a rheumatologist.
To cite this abstract in AMA style:
Snoeck Henkemans S, de Jong P, Luime J, Kok M, Tchetverikov i, van der Helm-van Mil A, vis m. The Window of Opportunity in Psoriatic Arthritis: Similar to Rheumatoid Arthritis? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-window-of-opportunity-in-psoriatic-arthritis-similar-to-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-window-of-opportunity-in-psoriatic-arthritis-similar-to-rheumatoid-arthritis/