Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Salivary gland (SG) ultrasound (US) helps to diagnose and stratify patients with Sjögren’s disease (SjD). However, US studies evaluating morphological changes over time are scarce. Therefore, we aimed to evaluate the potential progression of US morphological changes of SG in a well-defined SjD cohort.
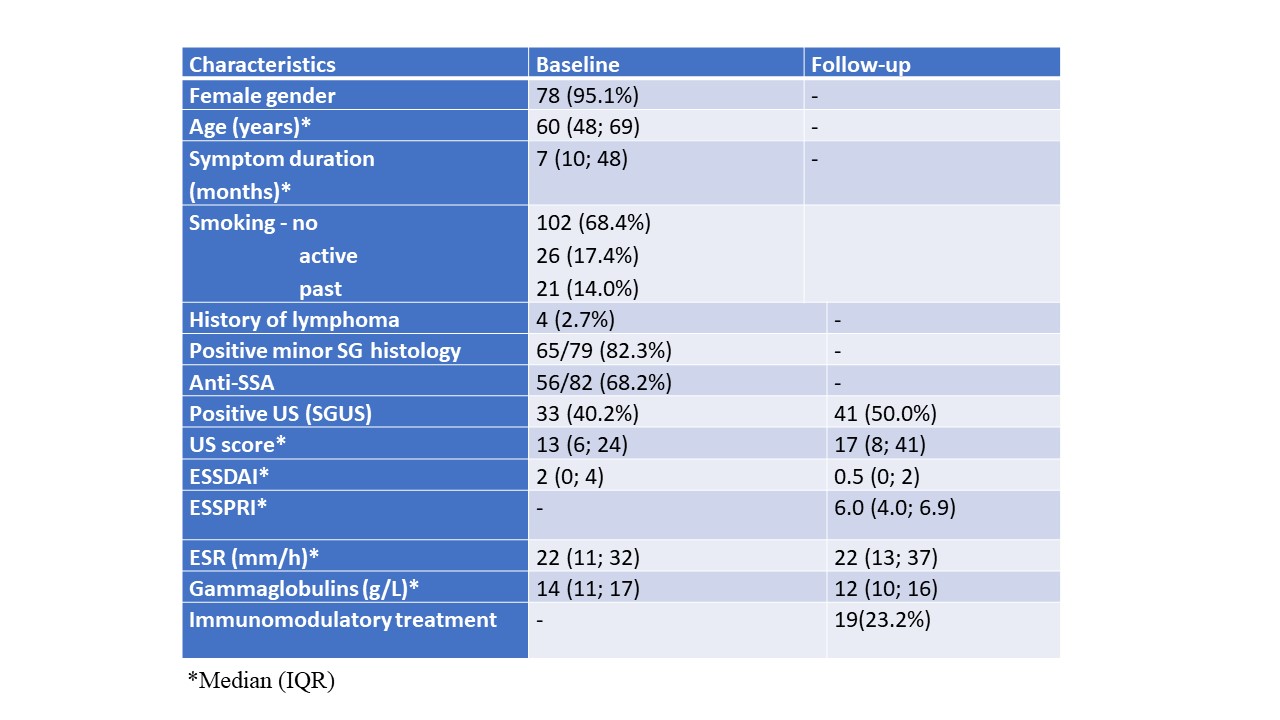
Methods: One hundred and fifty-one SjD patients diagnosed between January 2016 and December 2018, and fulfilling the ACR/EULAR 2016 classification criteria1 were invited to participate in a follow- up (FU) US study that was carried out between May and September 2023. In 82 out of 151 patients who responded to the invitation, the follow-up time (median (IQR)) was 73.1 (63.6, 81.3) months. A detailed clinical and laboratory evaluation, Schirmer’s test, SGUS using Hočevar scoring system2, and ESSDAI were repeated, and ESSPRI calculated. For the purpose of the study, a cut-off for significant US progression was set at US score change >12 points (from baseline).
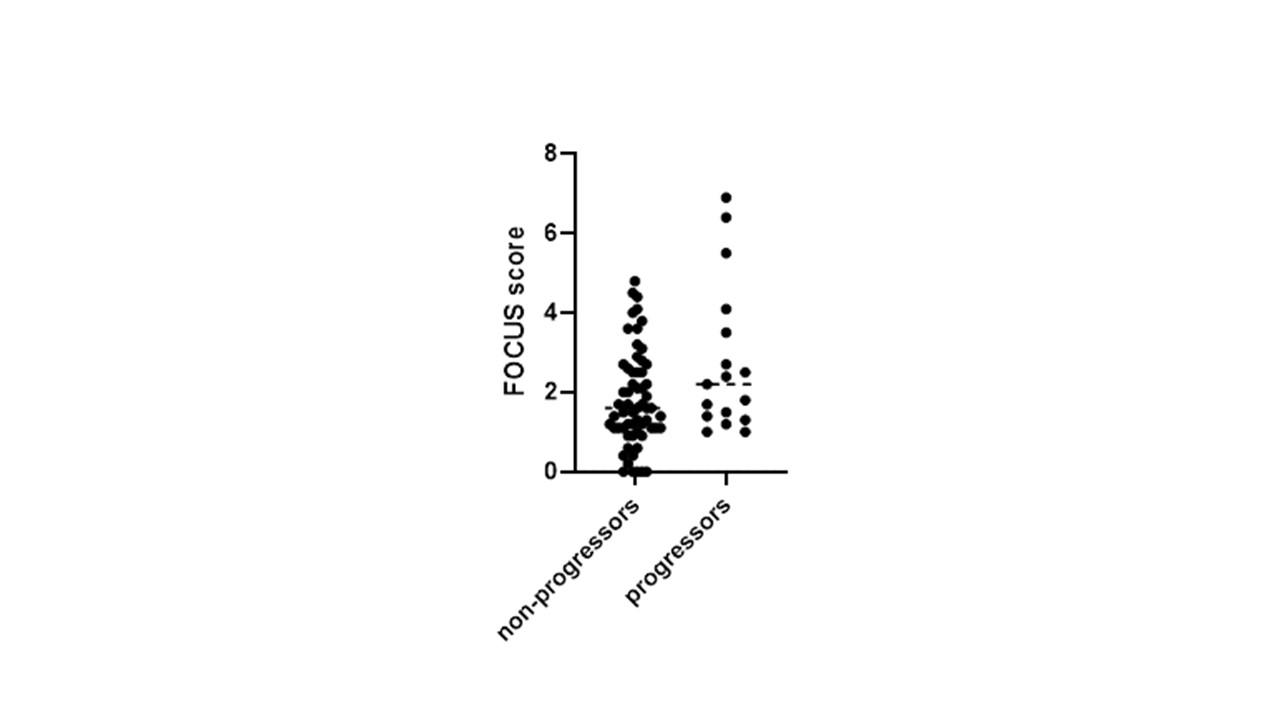
Results: Patients’ baseline characteristics are presented in Table 1. At FU visit 43 (52.4%) and 42 (51.2%) patients reported worsening of ocular and oral sicca symptoms. Median ESSPRI at FU was 6.0 (4.0; 6.9) and was at least 5 in 53 (64.6%) patients. There were no significant changes in ESR, gamma globulin level and ESSDAI compared to baseline. None of the included patients developed a new lymphoma during FU. At FU visit 41 (50.0%) patients had US changes consistent with SjD (at baseline 33 (40.2%)). According to the definition, significant increase of US score was found in 18 (21.9%) patients compared to baseline. We found no significant differences in patient age (p=0.516), symptom duration, time (p=0.222), oral dryness (p=1.0), glandular swelling (p=0.722), ESR (p=0.423), gamma globulins (p=0.617), baseline ESSDAI (p=0.352), follow-up ESSPRI (p=0.384) or immunomodulatory treatment (p=1.0) in patients with and without SGUS progression. There was a trend toward higher minor salivary gland focus score in those who US progressed (p=0.091; Fig 1).
Conclusion: Most of the SjD patients in our cohort showed stable glandular disease based on US evaluation. However, one fifth of SjD patients had significant US morphological glandular progression; we found no firm association between patients baseline characteristics or disease activity and US glandular progression.
References:
1. Shiboski CH, et al. Arthritis Rheumatol 2017;69:35–45.
2. Hočevar A et al. Rheumatology 2005;44(6):768-72.
To cite this abstract in AMA style:
Perdan Pirkmajer K, Lakota K, Praprotnik S, Rotar Z, Hocevar A. The Value of Ultrasound to Follow Glandular Disease in Sjogren’s Disease Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-value-of-ultrasound-to-follow-glandular-disease-in-sjogrens-disease-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-value-of-ultrasound-to-follow-glandular-disease-in-sjogrens-disease-patients/