Session Information
Date: Sunday, October 26, 2025
Title: (0233–0279) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatologists are increasingly involved in the management of patients with severe manifestations of rheumatologic disease treated with Extracorporeal Membrane Oxygenation (ECMO). A 2020 systematic review, reviewing the use of ECMO in rheumatology from 1999 to 2018, found a survival rate of 93% (in 27 of 29 patients). The use of ECMO has steadily increased since then. This systematic review documents the current status of ECMO use in patients with complications of rheumatologic diseases.
Methods: A systematic review was conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines, covering studies from January 2019 to January 2025 (Figure 1). The initial search identified 2,695 studies from 4 different databases. Inclusion criteria included patients requiring ECMO for rheumatologic disease complications with documented outcomes. Studies were excluded if they lacked outcome data, were not published in English, letters to the editor, secondary sources, or ECMO for non-rheumatologic indications. Data extracted included patient characteristics, ECMO indications and details, therapy type, outcomes, and complications.
Results: A total of 145 studies were included in the final analysis, encompassing 734 patients who received ECMO. The average age of patients was 32.2 years (range: 7 weeks to 70 years), with 340 (46%) females. The most common indications for ECMO were diffuse alveolar hemorrhage, severe interstitial lung disease, myocarditis, cardiac arrest, and massive pulmonary embolism. The most frequent rheumatologic diagnoses were anti-neutrophil cytoplasmic antibody (ANCA) vasculitis, inflammatory myositis, systemic lupus erythematosus (SLE), anti-glomerular basement membrane disease, and antiphospholipid syndrome. There were 482 patients treated with venovenous (VV) ECMO, 236 with venoarterial (VA) ECMO, and 10 were transitioned between VA and VV. ECMO duration ranged from 1 day to 123 days. Common therapies included glucocorticoids, cyclophosphamide, and plasmapheresis. Infection was the most frequent complication during hospitalization. In terms of outcomes, 362 patients were successfully bridged to recovery, 54 patients underwent successful transplants and survived, 304 patients died, and 3 patients remained on ECMO at the time of publication.
Conclusion: ECMO remains a potential and viable option for the severe manifestations of rheumatologic disease, serving as a bridge to either recovery or transplant. In this review, 416 patients survived due to ECMO who likely would have otherwise died. Overall, ECMO provides significant survival benefits, allows for organ recovery, and serves as a bridge to additional therapies, especially when used early and in carefully selected patients.
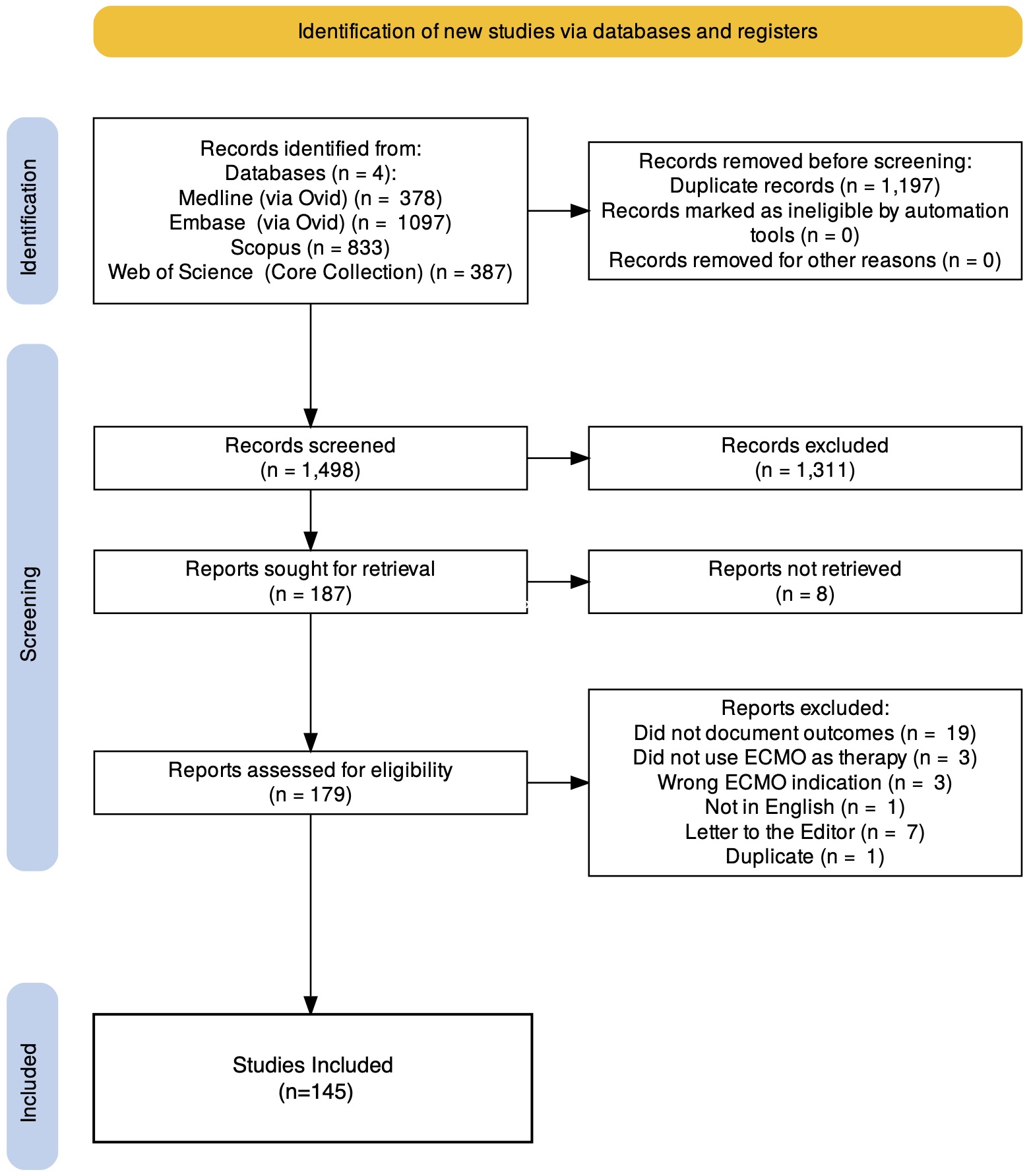 Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart outlining the process of screening and selection.
Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart outlining the process of screening and selection.
.jpg) Table 1. Summary of ECMO results (Part 1)
Table 1. Summary of ECMO results (Part 1)
.jpg) Table 1. Summary of ECMO results (Part 2 including glossary)
Table 1. Summary of ECMO results (Part 2 including glossary)
To cite this abstract in AMA style:
Falaas K, Tiegs L, Gertner E. The Role of Extracorporeal Membrane Oxygenation in Cardiopulmonary Dysfunction Due to Rheumatologic Diseases: A Systematic Review [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-role-of-extracorporeal-membrane-oxygenation-in-cardiopulmonary-dysfunction-due-to-rheumatologic-diseases-a-systematic-review/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-role-of-extracorporeal-membrane-oxygenation-in-cardiopulmonary-dysfunction-due-to-rheumatologic-diseases-a-systematic-review/
