Session Information
Date: Sunday, November 10, 2019
Title: 3S074: Epidemiology & Public Health I: Risk Factors & Outcomes for Rheumatic Diseases (821–826)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Venous thromboembolism (VTE, which includes pulmonary embolism [PE] and deep vein thrombosis [DVT]) is associated with increased morbidity and mortality. Previous studies have shown an increased risk of VTE in patients with psoriatic disease (PsD, which includes psoriasis and psoriatic arthritis) and rheumatoid arthritis (RA), two of the most prevalent inflammatory arthritis. However, population-based data using incident cohorts of PsD and RA are limited. Our objective was to estimate the risk of VTE, PE and DVT among patients with newly diagnosed PsD and RA compared with the general population.
Methods: We conducted a matched cohort analysis for PsD and RA separately. Our data included all outpatient and inpatient visits from Jan 1990 until Mar 2015 and all dispensed medication from Sept 1995 to Mar 2015 in the province of British Columbia. Incident PsD and RA patients were identified using previously validated algorithms and were matched with non-PsD (1:1) and non-RA (1:2) individuals randomly selected from the general population based on age, sex and entry cohort time. Patients should have at least a 7-year run-in period in order to consider the case as incident. Incident VTE was defined using ICD codes plus a dispensation of an oral anticoagulant. We calculated incidence rate ratio (IRRs), as well as age-, sex-, and entry-time-matched and multivariable hazard ratios (HRs) for the risk of VTE, PE, and DVT adjusting for potential confounders. To test the robustness of our results, we performed two sensitivity analyses. First, to estimate the effect of unmeasured confounders, we included a simulated unmeasured confounder into our model. Second, we accounted for the competing risk of death via the subdistribution proportional hazards model.
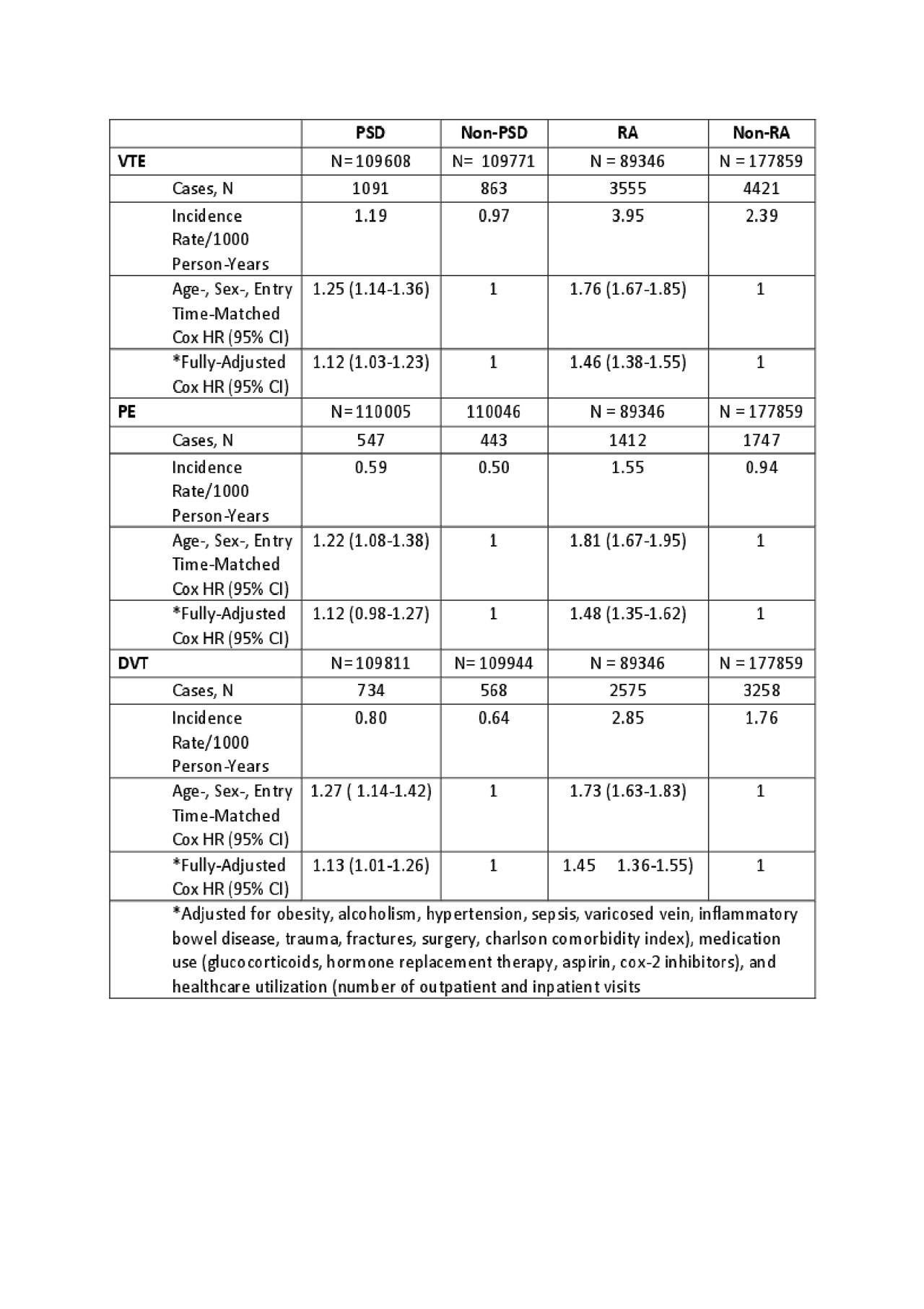
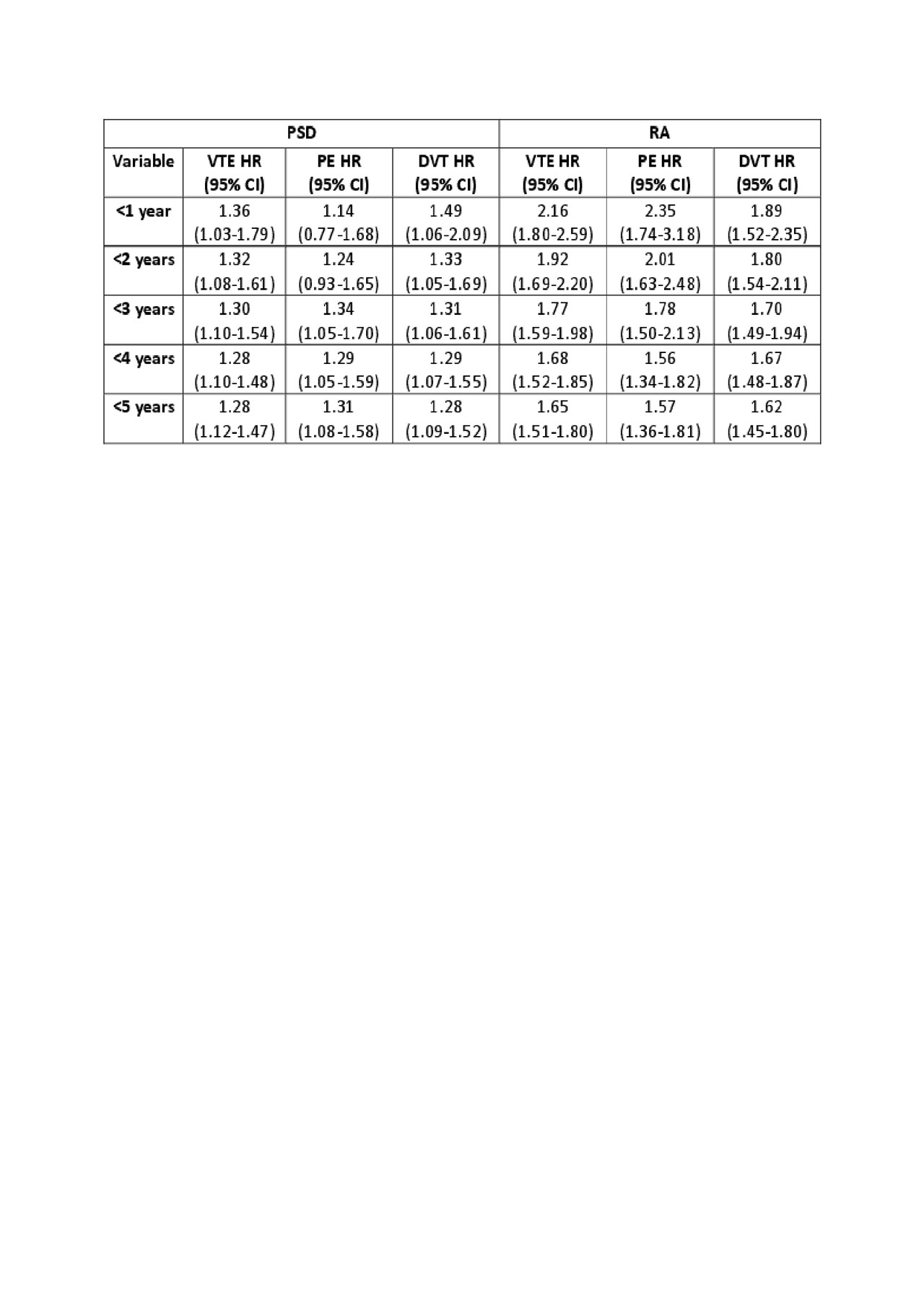
Results: Cohorts included 110,323 individuals with incident PsD (51% female, mean age 47 yrs) and 89,346 individuals with incident RA (66% female, mean age 59 yrs). Of those at risk of incident events, 1,091 and 3,555 developed VTE, 547 and 1412 developed PE, 734 and 2,575 developed DVT, respectively (incidence rates= 1.19 and 3.95 for VTE, 0.59 and 1.55 for PE, 0.80 and 2.85 for DVT per 1000 person-years, respectively). Compared with the corresponding non-PsD and non-RA cohorts the age-, sex-, and entry-time-matched HRs for VTE, PE and DVT were 1.25 and 1.76, 1.22 and 1.81, 1.27 and 1.73, respectively (P< 0.05 for all). After further adjustment for baseline characteristics, the HRs remained significant except for PE in the PsD cohort. The risks were greatest within the first year after diagnosis and progressively attenuated with time except for PE in the PsD cohort. HRs remained significant after accounting for the competing risk of death for all outcomes in both PsD and RA cohorts. The results also remained significant at values of 20% prevalence in the RA cohort and OR of 1.3 for the association between the unmeasured confounder and all outcomes, but not in the PsD cohort.
Conclusion: Patients with PsD and RA have an increased risk of VTE (12% and 46%), PE (12% and 48%) and DVT (13% and 45%). The risk of VTE peaked in the first year after diagnosis and decreased with time thereafter. These findings support the need of increased monitoring of VTE complications in patients with PsD or RA.
To cite this abstract in AMA style:
Li L, Lu N, Sayre E, Xie H, Lacaille D, Esdaile J, Avina-Zubieta J. The Risk of Venous Thromboembolism in Patients with Psoriatic Disease and Rheumatoid Arthritis, a Population-based Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-risk-of-venous-thromboembolism-in-patients-with-psoriatic-disease-and-rheumatoid-arthritis-a-population-based-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-risk-of-venous-thromboembolism-in-patients-with-psoriatic-disease-and-rheumatoid-arthritis-a-population-based-study/