Session Information
Date: Sunday, November 8, 2015
Title: Osteoarthritis - Clinical Aspects: Treatments and Epidemiology
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Symptomatic osteoarthritis (OA) and cardiovascular
disease (CVD) commonly co-exist. Our aim was to determine the extent to which
this relationship is explained by common risk factors (age and obesity),
metabolic factors and self-reported functional limitations.
Methods:
A population cohort aged ³55 years was recruited from
1996-98 from two communities. Age, sex, height and weight, self-reported medical
comorbidities, joint complaints and functional limitations (difficulty with
stair climbing, walking, and gripping) were collected by survey. Subjects with
inflammatory arthritis, rheumatic disease and medical neurological conditions
associated with functional disability were excluded. OA was defined as (1) swelling,
pain, or stiffness in any joint lasting 6 weeks in the past 3 months; and (2)
indication on the homunculus that a knee, hand and/or hip was “troublesome”. CVD
was defined as self-reported angina, heart disease, myocardial infarction,
coronary reperfusion, heart failure, stroke, transient ischemic
attack and/or carotid disease. Participants were classified into
8 mutually exclusive joint groups based on the presence/absence of knee, hand and
hip complaints. Using logistic regression, we examined the relationship of CVD
with knee, hand, and hip complaints, controlling for the following variables
added to our model incrementally: (1) age and body mass index (BMI); (2) sex
and metabolic factors (diabetes, hypertension and dyslipidemia); and (3) functional
limitations (stairs, walking, grip).
Results:
20,501 participants were included: mean age
68.2±8.5 years, 58.5% female, 51.8% rural-dwelling and mean BMI of 25.9±4.5
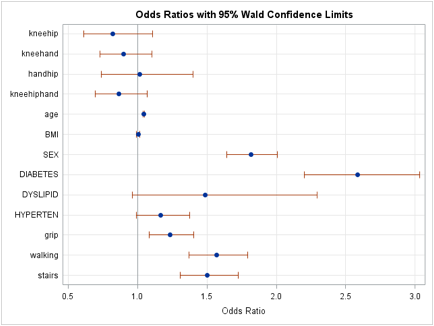
kg/m2. Controlling for age and BMI, the prevalence of self-reported
CVD was significantly higher among individuals with a combination of knee, hand
and hip OA (adj odds ratio [OR] 1.42, 1.16 –
1.72, p<0.01); combination of knee and hand OA (adj
OR 1.37, 1.13 – 1.66, p<0.01); and combination of hand and hip OA (adj OR 1.46, 1.07 – 1.97, p=0.02). Further adjustment
for sex and metabolic factors did not substantially impact these relationships.
When functional limitations were entered into the model, the above associations
were attenuated and became non-significant (Figure 1).
Conclusion:
In a large population cohort aged ³55 years, the previously documented relationship
between symptomatic OA (knee, hand, hip) and CVD was confirmed. This
relationship remained robust after controlling for common risk factors and metabolic
factors, but became non-significant after controlling for functional limitations,
suggesting that the predominant mechanism driving cardiovascular risk in people
with OA is functional disability. Further work is needed to investigate effective
ways to improve functional limitations in people with established OA.
Figure
1: Correlates of Self-Reported CVD by Multivariable Logistic Regression Model
To cite this abstract in AMA style:
King L, Kendzerska T, Hawker G. The Relationship Between Osteoarthritis and Cardiovascular Disease: Results from a Population-Based Cohort [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/the-relationship-between-osteoarthritis-and-cardiovascular-disease-results-from-a-population-based-cohort/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-relationship-between-osteoarthritis-and-cardiovascular-disease-results-from-a-population-based-cohort/