Session Information
Session Type: Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Autoimmune rheumatic diseases (ARD) such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) are salient causes of disability, functional limitations, reduced quality of life and increased mortality. Pain remains the chief complaint among patients with ARD despite the advent of more effective therapies. Current guidelines recommend prioritizing non-opioid treatments in chronic pain. However, little is known about recent changes in the use of chronic pain treatment modalities in ARD. Such knowledge will be foundational for updating chronic pain treatment guidelines in rheumatology. The aim of this study is to examine annual trends among a national sample of privately insured adults diagnosed with ARD.
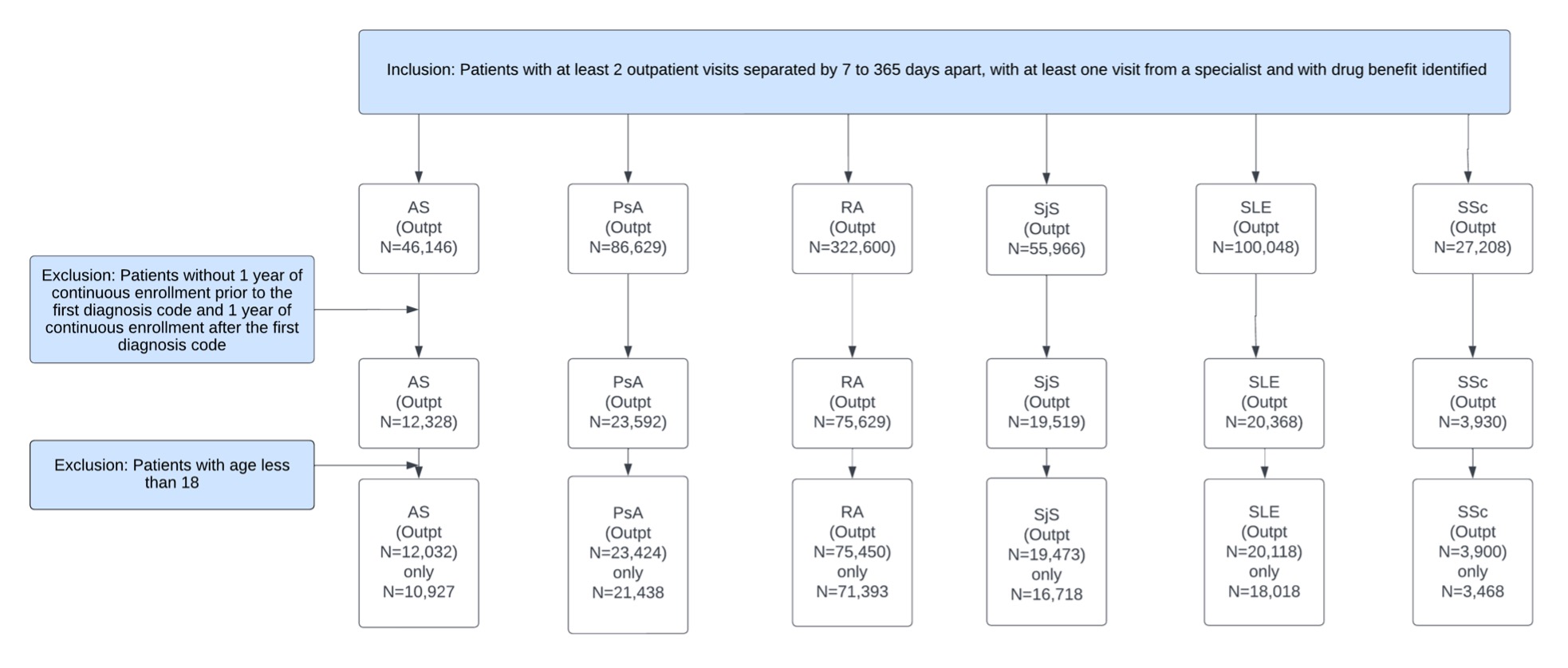
Methods: We used the IBM MarketScan Database (2007-2021) to identify patients in outpatient settings with ≥1 ARD diagnosis code by a specialist for ankylosing spondylitis (AS), psoriatic arthritis (PsA), RA, Sjogren’s syndrome (SjS), systemic sclerosis (SSc), and SLE. Our primary outcome was opioid use and secondary outcomes were use of anticonvulsants, antidepressants, skeletal muscle relaxants, NSAIDS, topical pain medications and physical/occupational therapy. We extracted the proportion of patients who met the outcomes for each year. The numerator included patients receiving medications or non-pharmaceutical therapy within one year of their 1st ARD diagnosis. The denominator included patients with their 1st ARD diagnosis. We used logistic regression to estimate the association between calendar time and outcomes, adjusted for age, sex, and region. We included a spline knot to balance model fit by maximizing model likelihood and interpretation of results.
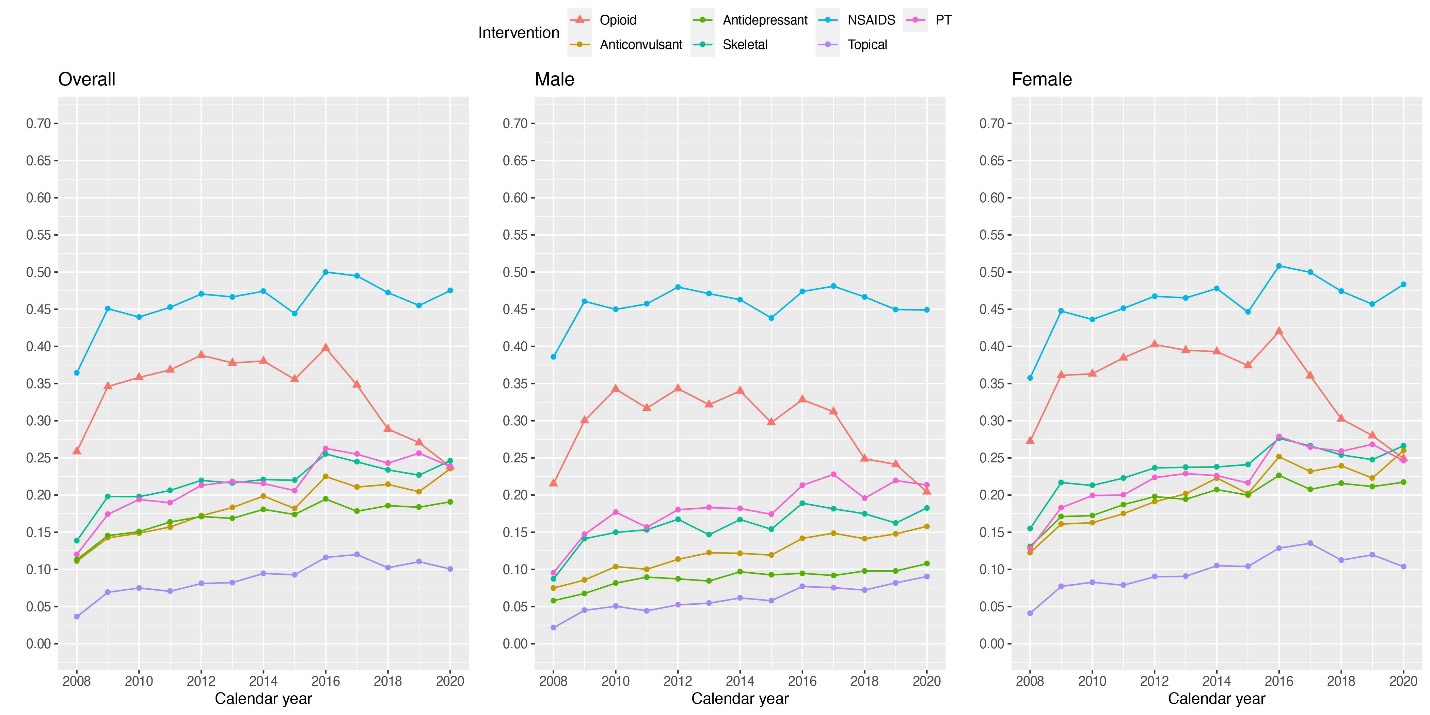
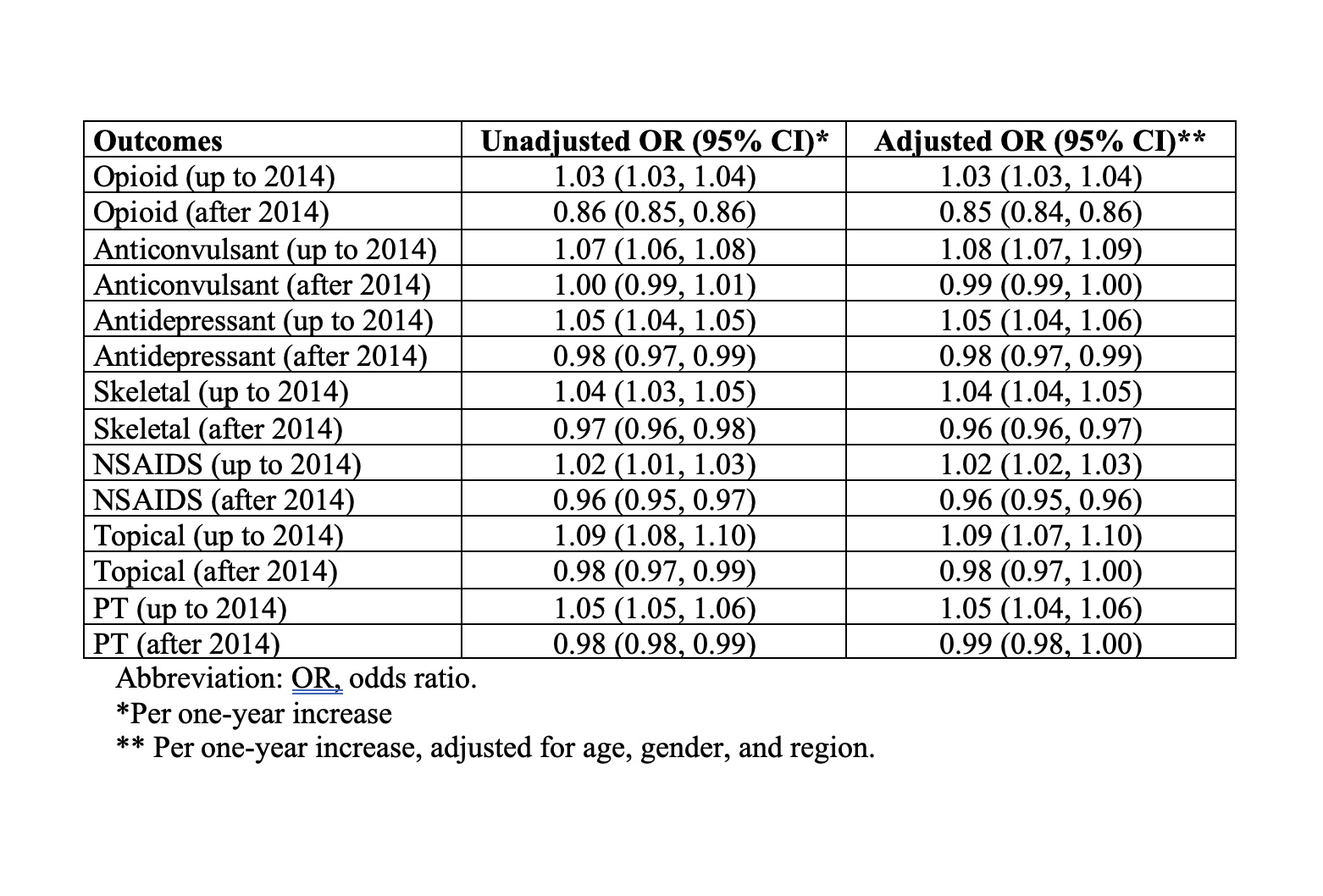
Results: There were 141,962 patients in our study (AS [n=10,927], PsA [n=21,438], RA [n=71,393], SjS [n=16,718], SLE [n=18,018], and SSc [n=3,468]) (Figure 1). Prevalence of opioid use increased from 26% in 2008 to 38% in 2014 and reduced to 24% in 2020. Prevalence of physical therapy use increased from 12% in 2008 to 24% in 2020. Prevalence of anticonvulsant use was 11% in 2008 and increased to 24% in 2020 (Figure 2). The odds of opioid use increased annually until 2014 by 3% [aOR, 1.03 (1.03, 1.04)] and decreased annually by 15% after 2014 [aOR, 0.85 (0.84, 0.86)] (Figure 3). The odds of physical therapy use increased annually by 5% until 2014 [aOR, 1.05 (1.04, 1.06)] and with a slight decrease annually by 1% after 2014 [aOR, 0.99 (0.98, 1.00)]. The odds of anticonvulsant use increased annually by 8% until 2014 [aOR, 1.08 (1.07, 1.09)], with no statistically significant time trend after 2014 (aOR, 0.99 (0.99, 1.00). The use of topical analgesics increased annually by 9% up to 2014 [aOR, 1.09 (1.07, 1.10)], while the use of NSAIDs decreased annually by 4% after 2014 [aOR, 0.96 (0.95, 0.96)]. These trends did not differ by gender except for NSAID use before 2014 and topical analgesic use after 2014.
Conclusion: The use of various nonopioid pain management modalities has increased or stabilized in recent years, while opioid and NSAID use has declined since 2014. Future studies are needed to evaluate the effectiveness of these changes, and what possible effects they have had on outcomes such as quality of life, disability, and function.
To cite this abstract in AMA style:
Falasinnu T, Lu D, Baker M. The Problem of Pain in Rheumatology: A Population-based Study of Annual Trends in Pain Management Modalities in Patients with Autoimmune Rheumatic Diseases in the United States, 2007-2021 [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-problem-of-pain-in-rheumatology-a-population-based-study-of-annual-trends-in-pain-management-modalities-in-patients-with-autoimmune-rheumatic-diseases-in-the-united-states-2007-2021/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-problem-of-pain-in-rheumatology-a-population-based-study-of-annual-trends-in-pain-management-modalities-in-patients-with-autoimmune-rheumatic-diseases-in-the-united-states-2007-2021/