Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Celiac disease (CD) is a gluten-sensitive enteropathy that develops in genetically predisposed individuals. Arthropathy has been reported as an extra-intestinal manifestation of CD. The pathogenesis of arthropathy is unclear; however, the immunologically mediated mucosal injury may lead to absorption of immune complexes or gut-derived antigens which may provoke antibody mediated autoimmune diseases including rheumatic diseases and arthropathy. We report a retrospective chart review of 35 confirmed cases of CD associated arthropathy and coexisting rheumatic or inflammatory disorders.
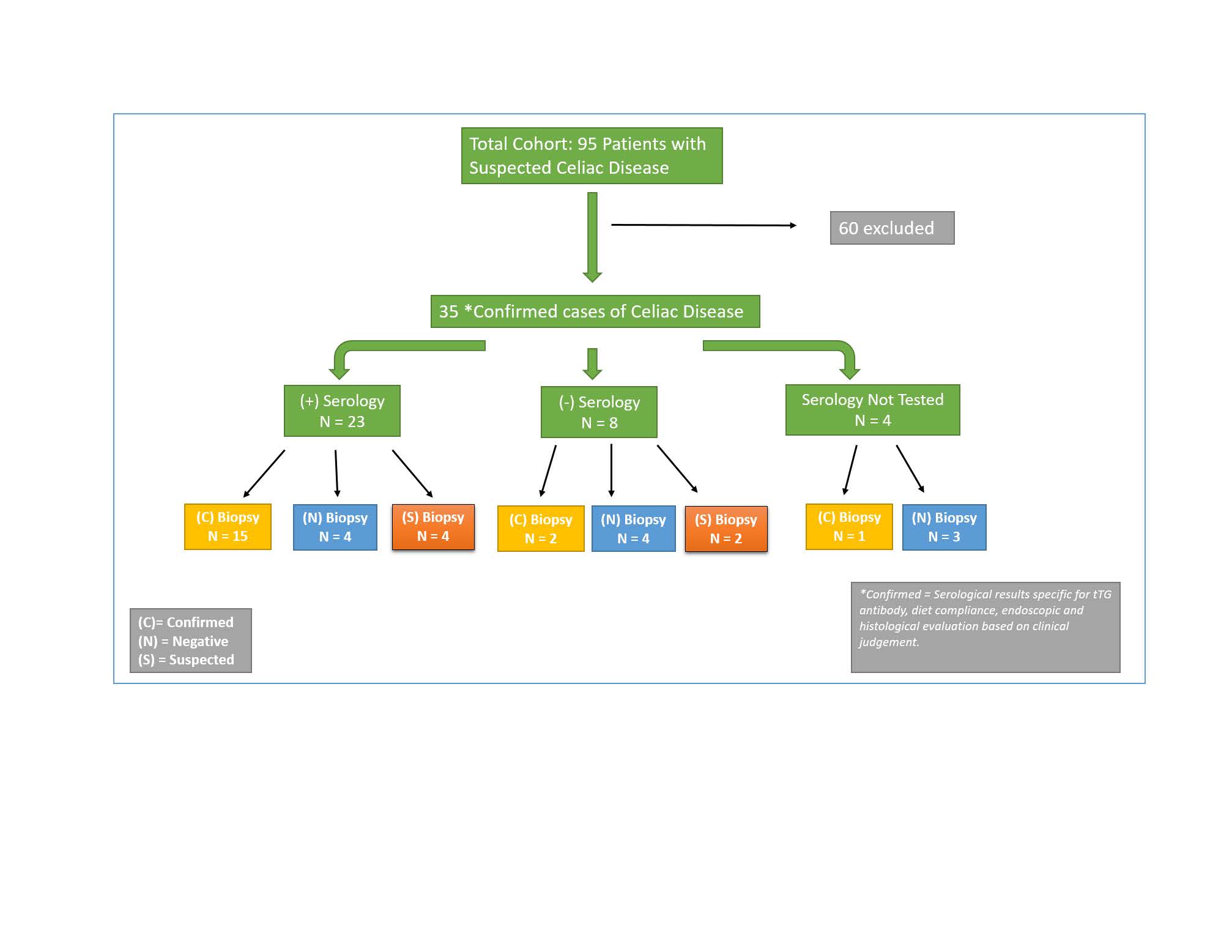
Methods: Heron database was used to search for patients seen by Gastroenterology and/or Rheumatology between January 2008 to January 2018 with suspected CD based on ICD-9 code for CD. These charts were retrospectively reviewed to determine who had confirmed CD, joint pain and pattern of involvement, dietary compliance, and other inflammatory or rheumatic disorders. The diagnosis of CD was based on serology specific for tissue transglutaminase (tTG) antibody, endoscopic and histological results, compliance with gluten free diet, and clinical judgement.
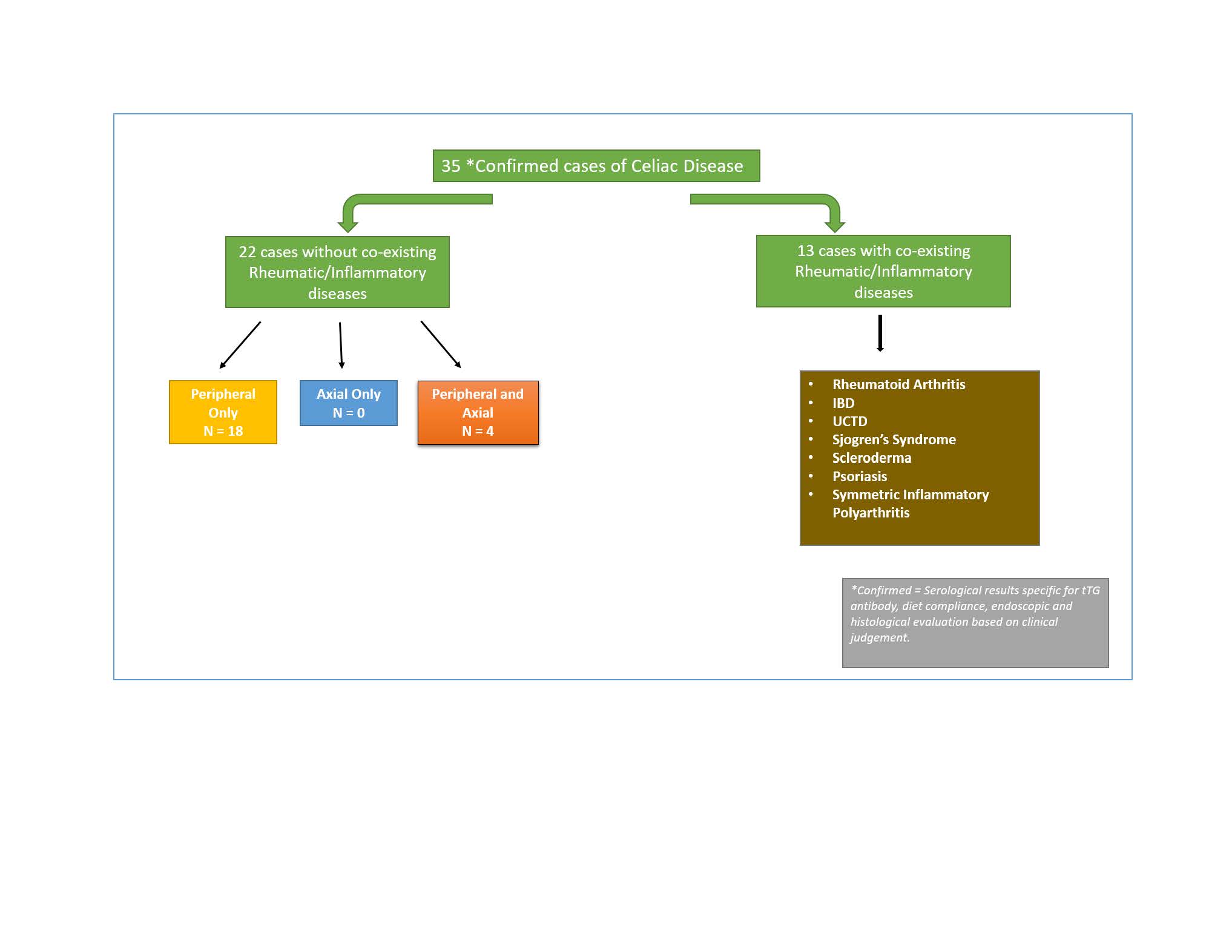
Results: A total of 95 patients with suspected CD were identified. 35/95 had confirmed CD. Of the 35 patients, 29 were female and 34 self-identified as Caucasian. The average age of patients was 49 years. Of the 35 patients, 22 patients did not have a co-existing rheumatic or inflammatory disorder. This cohort of 22 patients endorsed symptoms in the following distribution: 82% (18/22) had peripheral only, 0% (0/22) had axial only, and 18% (4/22) had peripheral and axial involvement. Of the 22 patients, 54% (14/22) endorsed arthropathy in small joints, 91% (20/22) in medium joints, and 82% (18/22) in large joints. Improvement in arthralgia after transitioning to a gluten-free diet was reported in 4/22 patients. A total of 13/35 with confirmed CD diagnosis had a rheumatic and/or inflammatory disorder. Rheumatoid Arthritis had the highest prevalence at 11% (4/35) followed by IBD (3), UCTD (2), Sjorgen’s Syndrome (1), Scleroderma (1), Symmetric Inflammatory Polyarthritis (1), and Psoriasis (1). Fibromyalgia, a non-inflammatory condition, was reported in 6% (2/35) of patients. 3 patients were not seen by rheumatology.
Conclusion: CD associated arthropathy and coexistence of CD with rheumatic and/or inflammatory disorders are under-recognized. Our data demonstrates that 63% of patients had CD associated arthropathy who appear to be a unique subset separate from those with coexisting CD and rheumatic/inflammatory disorders. Identifying the association and pattern of arthropathy in CD will aid in management of patients who either present to a gastroenterologist with extra-intestinal manifestations or to a rheumatologist with gastrointestinal manifestations. The awareness that CD can coexist in rheumatic diseases will aid rheumatologists in more effective recognition and management of patients with such presentations.
To cite this abstract in AMA style:
Moudgal A, Bhadbhade P, Haikal A, Maz M. The Prevalence and Patterns of Celiac Disease Associated Arthropathy and Coexistence of Celiac Disease with Rheumatic Disorders in a Single Tertiary Medical Center [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-prevalence-and-patterns-of-celiac-disease-associated-arthropathy-and-coexistence-of-celiac-disease-with-rheumatic-disorders-in-a-single-tertiary-medical-center/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-prevalence-and-patterns-of-celiac-disease-associated-arthropathy-and-coexistence-of-celiac-disease-with-rheumatic-disorders-in-a-single-tertiary-medical-center/