Session Information
Date: Tuesday, October 23, 2018
Title: Muscle Biology, Myositis and Myopathies Poster III: Treatment and Classification Criteria
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Although concomitant infectious diseases are the predominant causes of death in patients with polymyositis (PM)/dermatomyositis (DM), intensive immunosuppressive treatment are necessary for severe cases. We have already reported that high initial dose of glucocorticoid and combination immunosuppressive therapy for induction therapy, and KL-6 levels at the baseline were independent risk factors for infection. Here we investigated the predictive risk factors for opportunistic infection during immunosuppressive treatment for PM/DM by assessing cytomegalovirus (CMV) antigen test as a barometer for immunocompromised status.
Methods: We retrospectively analyzed clinical features, laboratory data at baseline in the patients with PM/DM who had received initial treatment at six hospitals affiliated to Yokohama City University from 2003 to 2016. We also investigated initial therapeutic regimens and clinical outcomes including CMV antigenemia as a complication. We conducted univariate and multivariate analyses to extract risk factors for CMV antigenemia.
Results: One hundred sixty-eight (PM 42, DM 82, and clinically amyopathic DM (CADM) 44) were recruited. The mean age was 56 ± 16 years and 120 (71.4%) were female. As initial therapies, oral prednisolone (PSL) was prescribed in all patients. Methylprednisolone (mPSL) pulse, intravenous cyclophosphamide (IVCY), and oral calcineurin inhibitor therapies were performed in 93 (56%), 50 (30%) and 86 (51%), respectively. Forty patients (24%) received combination therapy with IVCY and a calcineurin inhibitor. Fifty-two patients (31%) had CMV antigenemia within 6 months from initiation of immunosuppressant. An univariate analysis showed complication of ILD, high activity of ILD such as high KL-6 and low PaCO2 and strong immunosuppressive therapy tended to be positive CMV antigenemia (Table 1). There was no association between the cumulative PSL dose except within one month and CMV antigenemia. A multivariate logistic regression analyses revealed that low PaCO2 (p = 0.023, OR 0.78) and old age (p = 0.040, OR 1.07) were independent risk factors for CMV antigenemia. Moreover, the patients with positive CMV antigenemia tended to infected which were needed antibiotic therapy with significant differences (OR 4.52, p < 0.001). There were no patients with organ dysfunction as CMV infection.
Conclusion:
Although rapid and intensive therapies are required for PM/DM, appropriate monitoring, prophylaxis and early treatment for opportunistic infection are important, especially in patients who receive strong immunosuppressive therapy and who show low PaCO2 level and old age at baseline.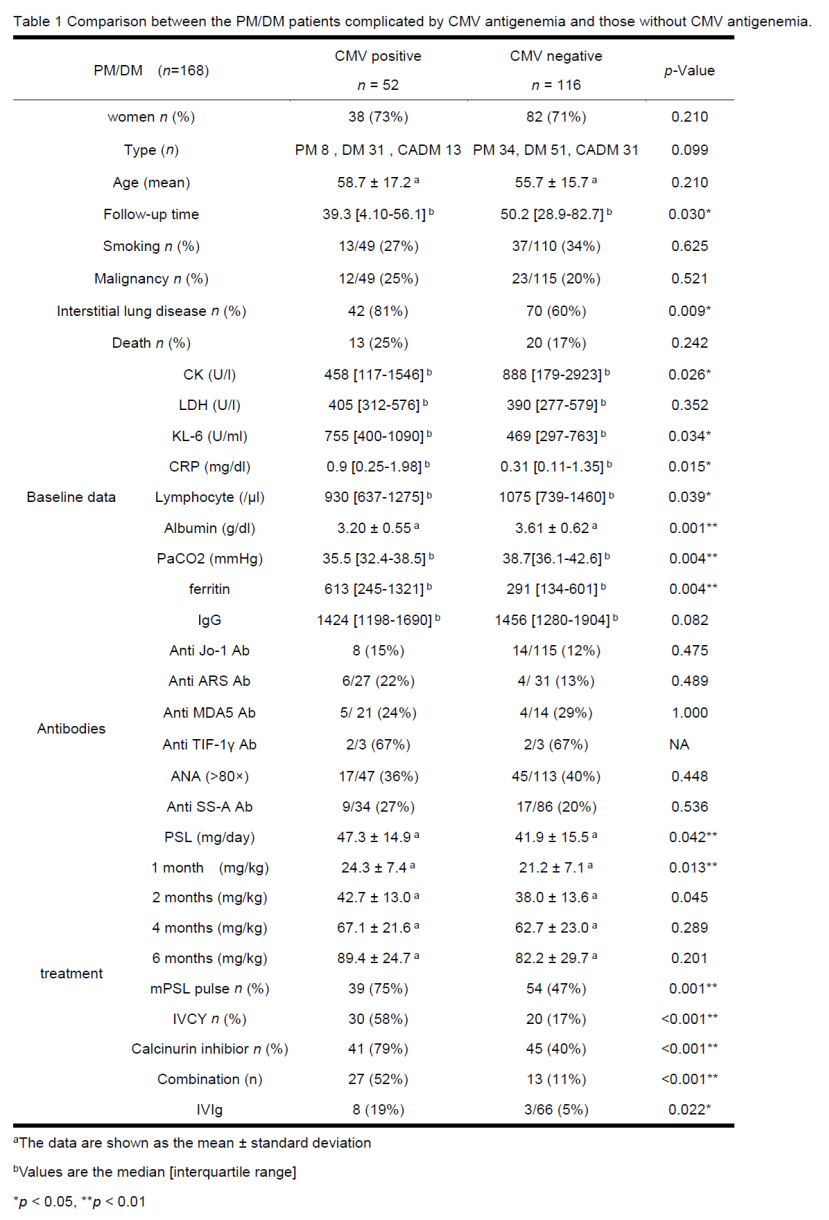
To cite this abstract in AMA style:
Sugiyama Y, Yoshimi R, Tamura M, Takeno M, Kirino Y, Ohno S, Nakajima H. The Predictive Risk Factors for Opportunistic Infection during Immunosuppressive Therapy for Polymyositis/Dermatomyositis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/the-predictive-risk-factors-for-opportunistic-infection-during-immunosuppressive-therapy-for-polymyositis-dermatomyositis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-predictive-risk-factors-for-opportunistic-infection-during-immunosuppressive-therapy-for-polymyositis-dermatomyositis/
