Session Information
Date: Wednesday, November 8, 2017
Title: Rheumatoid Arthritis – Clinical Aspects VI: Comorbidities of Rheumatoid Arthritis
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: The oral pathogen Aggregatibacter actinomycetemcomitans (Aa) generates citrullinated proteins targeted by autoantibodies in RA through its pore-forming toxin leukotoxin A (LtxA). Aa-derived LtxA is implicated in atherogenesis and atherosclerotic plaque instability, conditions over-represented in RA. No prior studies have explored the potential link between Aa, Aa-derived LtxA, and atherosclerosis in RA.
Methods: RA patients underwent cardiac computed tomography (CT) with coronary arterial calcification (CAC), a measure of coronary atherosclerosis, assessed. Serum levels of IgG antibodies against Aa serotype b and purified LtxA were measured by ELISA. Healthy controls cutoffs for seropositivity were used. Multivariable robust regression was used to model the associations of anti-Aa and anti-LtxA with CAC, adjusting for pertinent confounders.
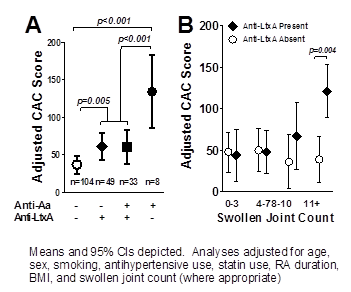
Results: A total of 194 RA patients [mean age=59 years; 60% female: median RA duration=9 years; 79% RF or anti-CCP seropositive] were studied. Anti-Aa was detected in n=41 (21%) and anti-LtxA in n=82 (42%). Adjusting for relevant confounders (listed in Fig), those with anti-LtxA had a mean CAC score 65% higher than those without anti-Aa or anti-LtxA (61 vs. 37 units, respectively; p=0.005 (Fig1a)]. Those anti-Aa+/anti-LtxA– had a mean adjusted CAC score 262% higher than those with neither antibody (134 vs. 37 units, respectively; p<0.001) and 120% higher than those with anti-LtxA, with or without concomitant anti-Aa. Among CAC-associated features, swollen joint count (SJC) was differentially associated with CAC depending on the context of anti-LtxA. In anti-LtxA– patients, SJC was not associated with CAC (Figure 1B, open circles). However, in anti-LtxA+ patients, each swollen joint was associated, on average, with a 6 unit higher CAC score (p<0.001). The interaction of anti-LtxA and swollen joints was significant (p=0.002). The association was not linear, with a marked difference noted in those with>10 swollen joints (Figure 1B, solid diamonds). Combining the two above groups with higher CAC scores [i.e. anti-Aa+/anti-LtxA– and anti-LtxA+ and>10 swollen joints; n=32 (16% of the cohort)], the adjusted mean CAC was 171% higher vs. those without these features (114 vs. 42 units, respectively; p<0.001).
Conclusion: Infection with the periodontal pathogen Aa may contribute to atherosclerosis in RA. Anti-LtxA, a marker of exposure to leukotoxic Aa strains, was significantly associated with more CAC and identified patients in which synovitis was robustly and independently associated with the extent of CAC. A subgroup of RA patients with isolated antibody positivity to the leukotoxic Aa serotype b showed markedly higher risk of atherosclerosis. Additional studies are warranted to elucidate the underlying mechanism, and whether Aa-specific screening and treatment may reduce CVD risk in RA patients.
To cite this abstract in AMA style:
Giles JT, Reinholdt J, Bathon J, Andrade F, Konig MF. the Periodontal Pathogen Aggregatibacter Actinomycetemcomitans Is Associated with Subclinical Coronary Atherosclerosis in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/the-periodontal-pathogen-aggregatibacter-actinomycetemcomitans-is-associated-with-subclinical-coronary-atherosclerosis-in-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-periodontal-pathogen-aggregatibacter-actinomycetemcomitans-is-associated-with-subclinical-coronary-atherosclerosis-in-rheumatoid-arthritis/