Session Information
Date: Monday, November 11, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster II: Treatments, Outcomes, & Measures
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Previous studies have shown that it is possible to taper DMARDs in RA patients with an inactive disease, but this is accompanied with a higher chance of disease flares. Current recommendations advise to taper DMARDs from a clinical viewpoint. However, data on the feasibility of tapering DMARDs from a patient’s perspective are sparse. Therefore, the objective of this study is to determine the impact and length of a disease flare, on patient reported outcome (PROs) in rheumatoid arthritis (RA) patients, who are tapering treatment.
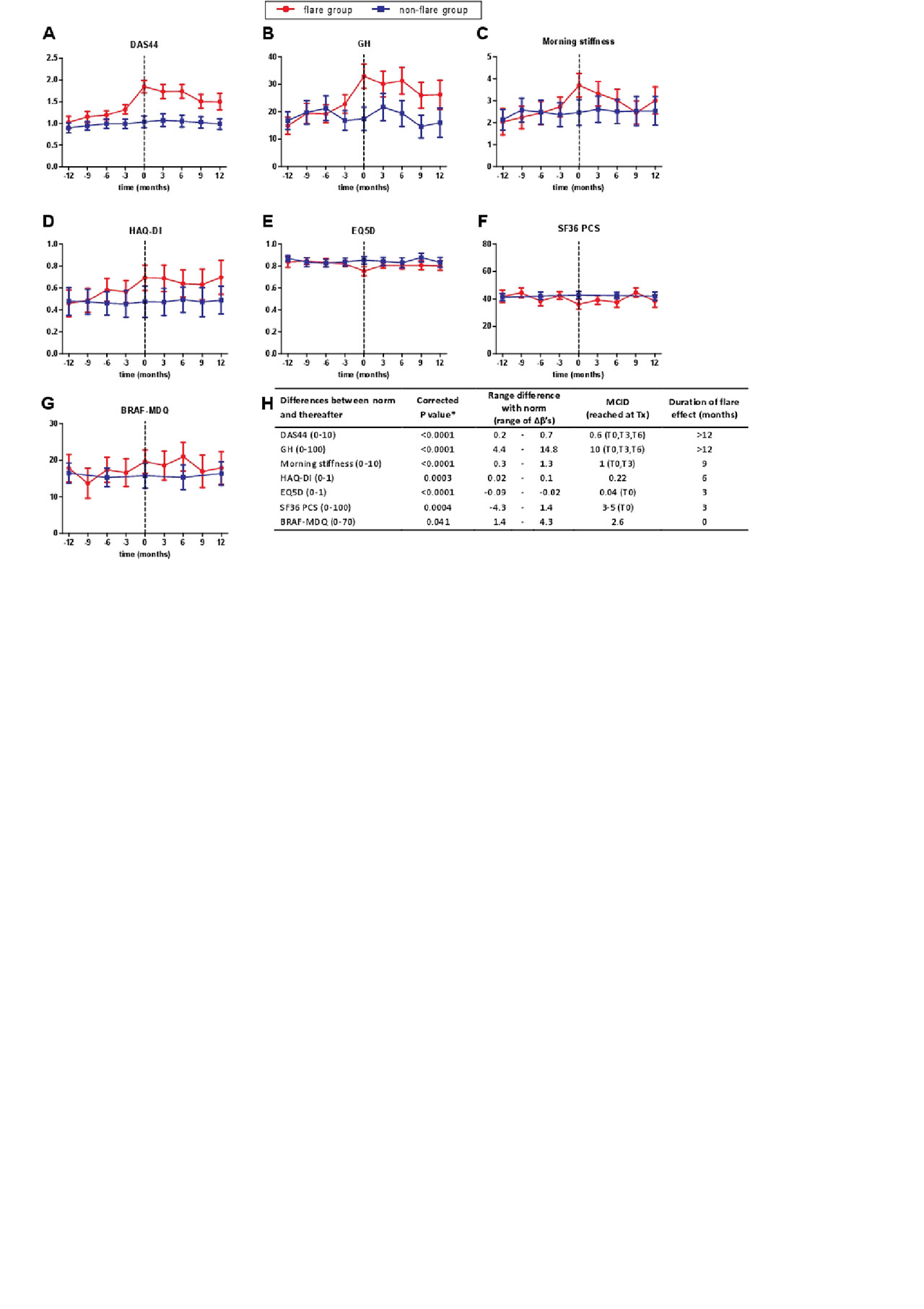
Methods: Data were used from the TARA trial; A multicenter, randomised controlled trial with well-controlled RA patients, DAS≤2.4 & SJC≤1, gradually tapering treatment. PROs of patients with a flare, DAS >2.4 or SJC >1, were compared at the moment of flare, 3 months prior to flare and every 3 months thereafter with their own norm. The norm was set at the average of DAS and PROs 12, 9 and 6 months prior to flare, which in our opinion was the best reference for well-controlled disease (figure 1A-G). Linear Mixed Models were used to determine within flaring patients if a flare altered DAS, VAS general health (GH), morning stiffness, functional ability (HAQ-DI), fatigue (BRAF-MDQ), quality of life (EQ-5D, SF36), anxiety and depression (HADS), and worker productivity over time, and if so, the duration was determined. For sick leave and unemployment we used descriptive statistics.
Results: In total, 113 patients experienced a flare. Patients who had a flare had a less stable course of the outcomes over time, compared with patients without a flare (Figure 1A-G). When comparing all time points to the norm, statistical significant differences were found for DAS (p< 0.0001), GH (p< 0.0001), morning stiffness (p< 0.0001), HAQ-DI (p=0.0003), EQ-5D (p< 0.0001), SF36 physical component scale (SF36-PCS) (p=0.0004), and the BRAF-MDQ (p=0.04) (Figure 1A-H). The DAS and GH significantly worsened at the moment of flare and this effect lasted >12 months. Morning stiffness and HAQ-DI worsened at the moment of flare and these PROs returned to their norm values 6 months thereafter (Figure 1H). The EQ5D and the SF36-PCS only worsened at the moment of flare. The BRAF-MDQ was not significantly different from the norm when comparing separate time points. For DAS, GH, morning stiffness, EQ-5D, SF36-PCS, and BRAF-MDQ the effect sizes were above the minimal clinically important difference (MCID) for >3 months (figure1H). Although the amount of sick leave increased from 1 to 1.3 days per month in the 6 months after flare and the worker productivity declined with 10% in the 3 months after a flare, these differences were not significant.
Conclusion: A disease flare influenced patients’ lives, which was mainly physical, and lasted at least 6 months. Although on a group level the effect size for each PRO is not always greater than the specific MCID, a disease flare can still be of great importance for the individual patient.
To cite this abstract in AMA style:
van Mulligen E, Weel A, Kuijper M, Hazes* M, van der Helm-van Mil A, de Jong P. The Patient’s Perspective on a Disease Flare During Tapering of DMARDs in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-patients-perspective-on-a-disease-flare-during-tapering-of-dmards-in-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-patients-perspective-on-a-disease-flare-during-tapering-of-dmards-in-rheumatoid-arthritis/